Dinah, ClinkShrink, & Roy produce Shrink Rap: a blog by Psychiatrists for Psychiatrists, interested bystanders are also welcome. A place to talk; no one has to listen.
Wednesday, August 24, 2011
An Anniversary to Forget
Over at Shrink Rap News on the Clinical Psychiatry News web page I've posted my latest rant about the Stanford prison experiment in recognition of its fortieth anniversary. Commenting over there is a nuisance, thus the post here. Pardon the inconvenience.
Sunday, July 10, 2011
No Better Than a Sugar Pill?
We're only a few minutes in to "today" but here's a link to an article in the New York Times by Peter Kramer-- In Defense of Antidepressants. Kramer writes:
Could this be true? Could drugs that are ingested by one in 10 Americans each year, drugs that have changed the way that mental illness is treated, really be a hoax, a mistake or a concept gone wrong?
This supposition is worrisome. Antidepressants work — ordinarily well, on a par with other medications doctors prescribe. Yes, certain researchers have questioned their efficacy in particular areas — sometimes, I believe, on the basis of shaky data. And yet, the notion that they aren’t effective in general is influencing treatment.
Kramer goes on to discuss issues in the research that may have biased studies that deem anti-depressants to be no better than placebo. Do read it if you get the chance.
Tuesday, March 16, 2010
Suicide and Social Learning
The author, Alex Mesoudi, used a computer model to study the effects of social learning and mass media influence on suicide clusters. He used a statistical method to see if suicides were clustered in time and space at an unexpectedly high frequency. This method is called an agent-based similiation, and is commonly used to model transmission of infectious disease. I'm not going to pretend to understand the statistics behind this! If you're curious you can read that part of the article.
He started by explaining the difference between point suicide clusters and mass clusters. Point clusters are suicides that are grouped together in time and space, while mass clusters are suicides that are grouped together in time, but are separated geographically. Suicide clusters have been thought to be due to social learning or mimicry, but it's also possible that they occur through homophiliy (the tendency for similar people to pool together in groups). Mass suicides are thought to be due to the influence of prestigious individuals (eg. celebrity suicide deaths) combined with coverage by the media. This leads to a one-to-many transmission model.
The computer model was run using three different assumptions: that suicides were totally random and unclustered, that clusters were due to social learning, and that clusters were due to homophily. He used different formulas to generate "suicides" under each model, and looked at the kind of clusters (spatiotemporal versus just temporal) that resulted.
What he found was that social learning caused spatiotemporal point clusters while homophilic clusters were more likely to be spacial rather than temporal. In order to understand this better, imagine the difference between teenage suicide epidemics versus correctional suicides. Teen suicides clusters happen among individuals who know each other, they happen in the same geographic area and within a short time frame of one another. These are the "social learning" clusters. Correctional suicides happen at a rate higher than in free society (in other words, they're geographically 'clustered' in a jail or prison), but are spread out over time. These are the homophilic suicides, in other words deaths by high risk people who happen to be grouped together. Based on this study, the correctional deaths are less likely to be due to social learning or mimicry.
Finally, the author studied the factors influencing mass suicide clusters: deaths that happen at the same time over a broad geographic area. These the kinds of suicides you see when a celebrity commits suicide. They are generally associated with a lot of media coverage. The computer model found that social learning played almost no role in these deaths.
It's a really complicated paper and I'm sure I didn't do it justice, but I thought it was pretty fascinating that someone could basically recreate the kind of suicide death patterns we see in the real world based on a theoretical mathematical framework. And I liked the term this author used for this kind of experiment: in silica. If in vivo experiments are done on animals or humans and in vitro experiments are done in test tubes or petri dishes, then "in silica" is a great term for computer model experiments.
And if none of this post made sense, hang on and I'll resurrect it in one of our podcasts.
Sunday, January 25, 2009
The Human Experiment, Part 2

Earlier this month, I posted about my own efforts to deal with insomnia, and how I inadvertently threw myself into caffeine withdrawal. I'm following up here.
So to summarize my experiment on myself, I manipulated the following variables, all at once, with no control group, and no way of knowing which variable was responsible for any changes I saw.
1) I stopped all caffeine. Well, mostly. After the caffeine withdrawal headache and fatigue, I decided there was no real rationale for this, and I've been drinking half a cup of coffee most mornings. In anticipation of the crowds and a purported 1:5000 person: porta-potty ratio at Obama's Inauguration, I did not have any coffee on that morning. I've had no Diet Coke (yes, this is possible) and my efforts to completely stop chocolate have been unsuccessful. So my caffeine intake has been limited to half a cup of coffee in the morning and episodic chocolate in reasonable (mostly) quantites. No artificial sweeteners.
2) I stopped drinking alcoholic beverages.
3) Since I have trouble falling asleep, but don't have trouble with daytime sleepiness, I wondered if I've simply come to need less sleep and I tried setting my alarm significantly earlier in the mornings. I am not a morning person, and this was awful (it lasted 2 days) but perhaps because it co-incided with my caffeine withdrawal. After that, I started going to bed at least an hour later than I was used to.
4) I increased the amount of exercise I was getting...oh, at least for a while. I also tried to add on some evening exercise to manipulate my body temperature several hours before bedtime-- a few minutes until I got flushed, but not sweaty enough to need a second shower. It was going well until a few days ago when I turned into a human slug. I resume a normal exercise schedule today.
5) Stress-- I started this plan during a time when stress was low and there was a long weekend in there. I've had some stuff going on since, and I spent a night away from home and my usual routine. Sometimes, life is just what it is.
My findings:
- It is easier to give up Diet Coke than it is to abstain from Chocolate.
- It is easier to give up alcohol than it is to abstain from chocolate.
- Decaffeinated tea is as happy an event as regular coffee.
- My daytime energy level has not changed with less morning coffee.
- One can actually have mild cravings for Diet Coke.
- It's easier to go to bed later than it is to get up earlier
- It's a pain in the neck to exercise every single day
- It is notably cheaper to eat in restaurants when there is no alcohol, soda, or after dinner beverage involved (I don't like decaf coffee).
Oh, and the results: most nights, I'm falling asleep within minutes and sleeping through the night.
Sweet Dreams!
Wednesday, July 30, 2008
Love Me, Love My Tats
 Recently one of our readers wondered what I thought of a study that was recently reported in Scientific American Mind. It was a study that was done in a forensic psychiatric hospital, looking at the correlation between tattoos and a diagnosis of antisocial personality disorder. Briefly, they examined 36 inpatients for the presence or abscence of tattos and then did semi-structured interviews to assess them for antisocial personality disorder. Unsurprisingly, they found that people with tattos were more likely to be diagnosed with antisocial personality disorder and to have histories of substance abuse and suicide attempts.
Recently one of our readers wondered what I thought of a study that was recently reported in Scientific American Mind. It was a study that was done in a forensic psychiatric hospital, looking at the correlation between tattoos and a diagnosis of antisocial personality disorder. Briefly, they examined 36 inpatients for the presence or abscence of tattos and then did semi-structured interviews to assess them for antisocial personality disorder. Unsurprisingly, they found that people with tattos were more likely to be diagnosed with antisocial personality disorder and to have histories of substance abuse and suicide attempts.
My first thought when I read this report was: "This was a forensic fellows' research project."
Psychiatrists in training to be forensic psychiatrists are encouraged to do some type of research project during their fellowship. Since the fellowship only lasts for a year, it can be difficult doing any kind of in-depth or groundbreaking studies. The tattoo project is not a ground-breaking study. The main reason it probably got published was because it was done on forensic inpatients (although Scientific American Mind confuses them with prisoners, they aren't). The research subjects were patients, not prisoners. They were committed to the hospital after being found legally insane (therefore, not a criminal at all) or incompetent to stand trial (mentally unfit to go to court, therefore their guilt is undetermined).
The most interesting aspect of this study was the one that was not addressed at all in the paper:
How did they determine that the patients, all of whom by definition were seriously mentally ill, were competent to give informed consent to a research project?
This question is at the cutting edge of forensic psychiatry these days, a field which is concerned with competency assessments and capacity for decision-making. There are particular ethical difficulties that arise when the research is being conducted on institutionalized subjects like patients and prisoners. I've already blogged about this in detail in my post Guinea Pigs Behind Bars. (Be sure to check out the link to the guinea pig costume web site. I still love it.)
You can download the entire study by clicking on the pdf link at the Wiley web site here.
Wednesday, October 10, 2007
Topamax Effective in Reducing Heavy Alcohol Drinking

This was a double-blind, placebo-controlled, 14-week study, using 371 study participants. Dose range was 50-300 mg daily. Side effects included tingling sensations, changes in taste, loss of appetite, and impairments in concentration. Mean daily dose was 171 mg/day. They started with 25 mg/d for Week 1, then 50 mg/day for week 2, and increasing by 50 mg weekly (in divided morning and night doses) to the maximum of 300 mg/d.
This may be a good approach to helping some people reduce drinking, especially folks who might also have bipolar disorder, which is sometimes also treated with Topamax.
"Our study had 3 limitations. First, while the pattern of adverse events was similar to that found in our previous study,3 the more rapid titration was associated with decreased study adherence with taking the medication. Previously, when topiramate was titrated over an additional 2 weeks (ie, over 8 weeks rather than 6 weeks), retention rates were similar between the topiramate and placebo groups. Clinical sites least familiar with topiramate experienced more difficulties with retention, whereas completion rates among some experienced groups approached 90% (data not shown). We advise clinicians to use the slower titration schedule and to provide participants with focused education on managing emergent adverse events to maximize adherence with taking the medication. Second, as with most clinical trials in the alcohol dependence field, enrolled participants have to meet criteria enabling the conduct of a safe study. Because this cohort is often relatively healthier and perhaps more homogeneous than the general population of all those seeking treatment for alcohol dependence, our ability to generalize without restriction from this trial to clinical practice is limited. Third, this study did not have a follow-up period, so we could not determine whether, how many, and at what interval participants would have relapsed following medication withdrawal. Nevertheless, with respect to how people fare, on average, following treatment for alcoholism in a clinical trial, a meta-analysis of recent studies has shown that, even after a single treatment event, most can show substantial reductions in drinking up to 1 year afterward.
Our finding in this study that topiramate is a safe and consistently efficacious medication for treating alcohol dependence is scientifically and clinically important. Alcoholism ranks third and fifth on the US and global burdens of disease, respectively. Discovering pharmacological agents such as topiramate that improve drinking outcomes can make a major contribution to global health. Because topiramate pharmacotherapy can be paired with a brief intervention deliverable by nonspecialist health practitioners, a next step would be to examine its efficacy in community practice settings."
Monday, October 08, 2007
Carbonated Panic Attacks
Panic attacks are an acute, dramatic form of anxiety, including symptoms of shortness of breath, lightheadedness, tingling sensation, and fear of impending doom. One of the theories about the biological basis of panic attacks is the false suffocation alarm theory proposed by Klein, which suggests that the brain's sensor that detects elevated carbon dioxide levels is overly sensitive in some people, triggering panic attacks for no clear reason.
Eric Griez, a psychiatrist from the Netherlands, has published an article in the open source, online journal PLOS One, demonstrating further evidence of this connection (see also review in Science Mag). He exposed volunteers without an anxiety disorder to high levels of carbon dioxide, thus triggering the suffocation alarm at appropriate levels of CO2.
 "Sixty-four healthy subjects underwent a double inhalation of four mixtures containing respectively 0, 9, 17.5 and 35% CO2 in compressed air, following a double blind, cross-over, randomized design. Affective responses were assessed according to DSM IV criteria for panic, using an Electronic Visual Analogue Scale and the Panic Symptom List. It was demonstrated that carbon dioxide challenges induced a dose dependent negative affect (p<0.0001).>
"Sixty-four healthy subjects underwent a double inhalation of four mixtures containing respectively 0, 9, 17.5 and 35% CO2 in compressed air, following a double blind, cross-over, randomized design. Affective responses were assessed according to DSM IV criteria for panic, using an Electronic Visual Analogue Scale and the Panic Symptom List. It was demonstrated that carbon dioxide challenges induced a dose dependent negative affect (p<0.0001).>
This falls under the what's-old-becomes-new-again category, as I recall this area of research 15 years ago. Still, it may be worth stirring up again, especially if it leads to more effective and safer treatments. In fact, Klein and Preter just published an amplification of the original theory, including evidence of involvement of opioid receptors in the response to the alarm being triggered.
Friday, August 24, 2007
Molecular Psychiatry: Schizophrenia Mouse Model

Here's another interesting knockout mouse model for schizophrenia. This was in the July 31 issue of Molecular Psychiatry, "Phospholipase C-1 knockout mice exhibit endophenotypes modeling schizophrenia which are rescued by environmental enrichment and clozapine administration," by McOmish et al., in Australia.
"Phospholipase C-1 (PLC-1) is a rate-limiting enzyme implicated in postnatal-cortical development and neuronal plasticity. PLC-1 transduces intracellular signals from specific muscarinic, glutamate and serotonin receptors, all of which have been implicated in the pathogenesis of schizophrenia. Here, we present data to show that PLC-1 knockout mice display locomotor hyperactivity, sensorimotor gating deficits as well as cognitive impairment. These changes in behavior are regarded as endophenotypes homologous to schizophrenia-like symptoms in rodents. Importantly, the locomotor hyperactivity and sensorimotor gating deficits in PLC-1 knockout mice are subject to beneficial modulation by environmental enrichment. Furthermore, clozapine but not haloperidol (atypical and typical antipsychotics, respectively) rescues the sensorimotor gating deficit in these animals, suggesting selective predictive validity. We also demonstrate a relationship between the beneficial effects of environmental enrichment and levels of M1/M4 muscarinic acetylcholine receptor binding in the neocortex and hippocampus. Thus we have demonstrated a novel mouse model, displaying disruption of multiple postsynaptic signals implicated in the pathogenesis of schizophrenia, a relevant behavioral phenotype and associated gene–environment interactions."PLC-1 is one of those proteins involved in processing the signal after the receptor is activated. Think of the ignition in your car. If the key is the neurotransmitter, like serotonin (or medication, like Prozac) and the lock (or keyhole) is the receptor, then PLC-1 is one of the wires that connects the lock on the steering column to the starter, which gets the engine going. We are all so used to thinking that what is important is the action at the receptor, but it is easy to forget that there is this whole other layer of machinery that gets engaged once the receptor is activated.
These so-called second messenger systems use a cascade of Rube Goldberg connectors to make things happen. Just like a genetic error can cause a receptor to malfunction, so can errors in this second messenger cascade.
This particular enzyme is involved in the growth and connectivity of brain cells. The researchers show that mice who are engineered to not produce PLC-ß-1 develop cognitive problems which have similarities to those seen in humans with schizophrenia. Changes in the environment can minimize these problems, suggesting that this animal model could be used to test other treatments -- including medications that work very differently from what is out there now -- for potential use in this neurodevelopmental illness.
Saturday, June 09, 2007
DBH Gene in Cocaine-Induced Paranoia
 So I thought I'd make another post about how more is being learned about our genetic makeup and how that may relate to medication side effects. In this instance, the "medication" is cocaine, which causes a huge release of dopamine. Some folks get really paranoid after using cocaine. This study asked the question "Is reduced breakdown of dopamine associated with paranoia symptoms in cocaine users?"
So I thought I'd make another post about how more is being learned about our genetic makeup and how that may relate to medication side effects. In this instance, the "medication" is cocaine, which causes a huge release of dopamine. Some folks get really paranoid after using cocaine. This study asked the question "Is reduced breakdown of dopamine associated with paranoia symptoms in cocaine users?"
First some background. The above graphic shows that the neurotransmitter dopamine (or DA) is converted into norepinephrine (or NE, sometimes also called noradrenaline, or NA) by the enzyme dopamine beta-hydroxylase (DBH). You can see that all this enzyme does is add the little -OH (or hydroxy) part to the dopamine molecule to make norepinephrine.
Kalayasiri 2007 showed that a particular mutation (C1021T) in the dopamine beta-hydroxylase (DBH) gene was associated with significantly increased paranoia in a small group of cocaine abusers (see top graph). Cocaine users were blindly provided with different doses of cocaine (bet it was easy to find subjects) and their level of paranoia was rated every few minutes using a Visual Analog Scale (VAS). Users with the TT variant of the gene rated their paranoia level consistently higher than those with the CC or CT gene variant. It has elsewhere been shown that the TT form of the DBH gene is broken, and so is much weaker at converting DA to NE. The resulting higher levels of dopamine in the TT people may be why they get more paranoia.
[Genetics 101 Note: when you see this type of notation, "C1021T", all it means is that at position 1021 along the double-stranded DNA for that particular gene, there is either a C or a T nucleotide at this single point on either DNA strand... if each of your two DNA strands (one from Mom, one from Dad) contain one or the other, then you are homozygous for either one (CC or TT)... if Mom gave you a C and Dad gave you a T, then you are a CT (called heterozygous). Thus there are 3 genetic variants (in this case, CC, CT, or TT) which can exist at this single nucleotide position. These single nucleotide variants, or "polymorphisms", are referred to as SNPs, or Single Nucleotide Polymorphisms. Different SNPs can result in that particular gene's product or function to be enhanced or diminished, resulting in functional variations which may contribute to individual variations in one's response to disease, drugs, or the environment.]
Because this paranoia and related symptoms are uncomfortable to most people, it may serve as a deterrent to using cocaine. In fact, folks with the TT genotype might be at reduced risk of becoming addicted to cocaine because their DBH gene does not work as well. In fact, the alcohol deterrent drug, disulfiram (Antabuse), also happens to block the DBH enzyme (remember, the DBH gene contains the instructions to make the DBH enzyme). This would result in someone with a normally functioning enzyme (from a CC or a CT SNP) to have an enzyme that works like someone with a TT SNP. Antabuse has been shown to be helpful in treating cocaine addiction.
As further evidence of this connection, Schank 2006 used DBH knockout mice to demonstrate hypersensitivity to cocaine in these animals, suggesting that low DBH activity in some cocaine abusers may increase the drug-related dysphoria and aversion, making them less likely to become addicted to the drug.
We hypothesize that the ratio of dopamine (DA) to norepinephrine within noradrenergic vesicles is elevated in TT [homozygous] subjects, so that during cocaine intoxication, DA-mediated neurotransmission is relatively elevated in regions richly innervated by noradrenergic and dopaminergic fibers (e.g., prefrontal cortex). Alternatively, given observations of up-regulated high affinity DA receptor binding sites in DBH knockout mice, TT homozygotes may be hypersensitive to DA, and thereby [may] be more vulnerable to cocaine-induced paranoia.
Pretty cool.
Friday, April 06, 2007
VEGF: the New antidepressant

They show in rats that:
- VEGF goes up with ECT, with an sSRI (fluoxetine/Prozac), and with an sNRI (desipramine/Norpramine)
- This increase in VEGF is associated with new neuronal growth in the hippocampus
- Treatment with ECT, fluoxetine, or desipramine is associated with new neuronal growth in the hippocampus
- Injecting VEGF is associated with an antidepressant response in animal models of depression
- Blockade of the VEGF receptor with Flk-1 blocks the growth of new neurons in the hippocampus (in all 4 experimental arms--ECT, fluoxetine, desipramine, or VEGF injection)
- Blockade of the VEGF receptor blocks the behavioral response to ECT, fluoxetine, or desipramine in animal models of depression
Thursday, March 08, 2007
Bridging the gap between research and change in practice
The Journal of the American Medical Association (JAMA) and the Institute for Healthcare Improvement (IHI) have initiated a collaboration, funded by a grant from the Robert Wood Johnson Foundation, that will make it easy for health care professionals to review and discuss research findings from recent JAMA articles with the author. The participants of this Author in the Room program will be surveyed later to determine the degree to which they have implemented appropriate chnages in their practice. Participation is free and is by conference call (you have to register). The March 21 program will be on "Development and Validation of Improved Algorithms for the Assessment of Global Cardiovascular Risk in Women: The Reynolds Risk Score."
This is different sort of program than just your average CME event. The goal is to learn something that can be applied today in your practice to improve the health of your patients.
I hope we start to see more of this type of collaboration and effort to translate research findings into current patient practice. I also hope that this process isn't hijacked by Big Pharma into another marketing avenue (though it would seem hard to prevent).
If I see that JAMA is doing one of these programs for a psychiatric illness, I will let you all know.
Saturday, December 16, 2006
What's Inside the Black Box? FDA Antidepressants Hearing, pt. 2
[posted by Roy]
A couple days ago, I reported on the results of the FDA Psychopharmacologic Drugs Advisory Committee's hearing on December 13, 2006, on the FDA's plan to add a black box warning about the increased risk of suicidality in young adults. (I tried to get this done earlier, but just didn't have the time.)
Here are some notes I made at the hearing...
Sheila Matthews, from AbleChild.org, suggested requiring MedWatch info on all pharmaceutical advertising. I think this is a great idea. MedWatch is the voluntary, side-effect reporting mechanism for the FDA. Few prescribers and fewer consumers use it to report side effects. They should go one further and make it very easy to report side effects... almost as easy as googling the side effects.
There were two out of state attorneys who brought a number of their clients to testify. There were also at least two people there testifying for the Church of Scient ology's C C H R (and making excellent points, I might add, about Lilly's reported lack of following through with their promise 15 years ago to provide additional data. There were quite a few who lost family members tragically after taking only several doses of medication. It is indeed hard to understand how a chemical can cause one to conduct such complex, planned behaviors. Yet, listening to their testimony, it was hard to wonder how their response to these antidepressants could not have contributed to their deaths.
Heidi Bryan, from the Feeling Blue Suicide Prevention Council, pointed out that a big part of the not-enough-follow-up problem was due to the lack of parity for mental health treatment. Even Medicare charges 2-1/2 times as much for co-payments for outpatient mental health diagnoses than they do for the same symptoms caused by non-psychiatric diagnoses (e.g., major depression vs hypothyroidism).
I think that managed care and pharma has so convinced folks that taking a pill is just as effective as talk therapy, that there is now a backlash that will soon require these companies to drop their discriminatory policies.
All of the voting committee members, including Wayne Goodman, Gail Griffith, George Armenteros, Andrew C. Leon, Marcia J. Slattery, Susan K. Schultz, Jean Bronstein, and the chair, Daniel S. Pine, repeatedly pointed out the importance of balancing any labeling changes with language which emphasizes the need to weigh the relative risks of nontreatment with those of treatment, even comparing the risk of treatment with that of non-treatment. In fact, when the vote came up about extending the language in the black box to include the young adults, two members voted against (Griffith and Pines), while the other six voted for it under the condition that balancing language be included as well. They told the FDA that they wanted to review the draft language prior to making a final decision.
Joe Glenmullen, who authored "Prozac Backlash", testified, as well. He and others state the the FDA has been tricked by the drug companies, by not being given complete information about all clinical trial results.
So, then the committee deliberated for a few hours. I must say, the committee members rather awkwardly, but repeatedly, made several important points...
- The FDA needs to make the drug companies collect and provide better data.
- There is inadequate data on this "activation syndrome", referring to akathisia, agitation, and anxiety apparently induced by antidepressants in some individuals.
- Collecting pharmacogenetic data might help in determining which individuals might be at higher risk of developing this and other side effects.
- The FDA is not collecting adequate data to differentiate between suicidal thoughts and suicidal behaviors and attempts. The pharmaceutical companies need to be directed to supply this type of fine-grained data. The fact that the currently reviewed data on "suicidality" makes it impossible to differentiate these two important characteristics suggests that any change in warning language needs to be carefully worded.
- The committee insisted on the FDA adding balancing language to reflect not only the increased risk of "suicidality" in young adults, but also the other side of the coin -- the increased risk associated with untreated depression. Additionally, they'd like language which refers to the apparent protective effect of these drugs in older adults, especially in seniors. It was noted that this would be the first time that the FDA has included in a black box information of a positive nature.
- They are concerned about the unintended consequences of decreased access to depression treatment as a result of the black box warning. Recent CDC information was noted, indicating that since the 2004 pediatric black box was added, prescriptions in kids are down, while suicides are up. This trend has already been noted in adults, and the fear is that it will only get worse with language that extends to young adults.
- The "25 to 30 year old" group mentioned in Part 1 was not chosen scientifically. It just fit the data. Thus, there is nothing special that happens when you turn 25 or when you turn 31to alter your risk. Because of this, they considered instead using language like "young adults", but this idea didn't seem to be too popular.
- Some of the possible explanations discussed for the biphasic nature of the data (higher risk when younger, lower risk when older) included induction of mania, late maturation of frontal lobes so impulsivity and experience improve as you get older, and greater tolerance for uncomfortable affect with age. They agreed that more data would be helpful.
- The committee also felt it was very important to emphasize the need for close follow-up when treating people of any age with depression. There was concern that it could sound like older people don't need to be followed as closely due to this "protective effect".
- Finally, the FDA acknowledged concern about telling doctors how to practice, and crossing the line into federal regulation of the practice of medicine. However, it was pointed out that, when the stakes are high enough, as with clozapine, the FDA has had no trouble advising things like frequency of monitoring lab tests. Telling prescribers that people with depression starting antidepressants should be followed at least weekly at first should be no different. Hopefully, they won't wimp out.
I'll leave you with two good quotes.
"Maybe we don't need a black box on antidepressants. Maybe we need a black box on Depression."
"How many will die with the black box? How many will die without it?"
technorati tags:FDA, depression, hearing, PDAC, antidepressants, suicide, suicidality, SSRIs, psychiatry, psychiatric, medication
Blogged with Flock
Thursday, December 14, 2006
FDA Hearing on Antidepressants, Depression, and Suicide

[Posted by Roy]
I attended yesterday's hearing, missing the FDA's presentation in the morning, but arriving for the public comments part and the afternoon deliberations. (Check out the FDA's 150-page .pdf testimony.) I was also among the 75 people who provided testimony to the committee. The meeting lasted a total of 9.5 hours!
This is the first time I've been to an FDA Advisory Committee meeting. These are public meetings (required to be public, by law) in which the committee members discuss the issues and make decisions. The FDA presents data to them; in this case, it was data from numerous clinical trials solicited from big pharma to especially get at the question of induction of suicidal thoughts or behaviors by antidepressant medications. After the committee hears these data, they listen to public testimony. After that, they discuss what they heard, and respond to the FDA's recommendations in the form of support, opposition, or other recommendations.
The committee is advisory in nature, meaning that the FDA takes what they say into consideration, but is not bound by their recommendations. The FDA does typically follow their recommendations. Three of the committee members could not vote due to conflicts of interest (receiving industry funds for clinical research and such).
In this post, I will first cut to the chase and tell you what the committee's recommendations were. In a second post, I'll give you more details to flesh out some of the discussion points and concerns that the committee raised, and also discuss the public testimony, some of it being very gut-wrenching and impassioned.
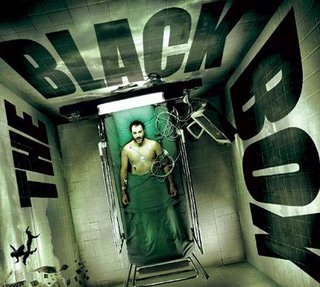
If I had to choose one image that best describes the entire hearing, it is the one above.
What this demonstrates is that as age goes up, the relative risk of suicidal thoughts or behavior goes down. The numbers plotted are the Odds Ratios... meaning that, compared to the folks taking placebo, what are the odds that those taking antidepressants are likely to have either thoughts of suicide or actual suicidal behavior. So, an O.R.=1 means that the chances are the same, which means no difference. An O.R.=2 means your chance is doubled. An O.R.=0.5 means your chance is halved. The black square is the estimated O.R., and the gray bar represents the 95% Confidence Interval... meaning that the statistical probability of the true O.R. being within the gray bar is 95%. Thus, if the gray bar touches 1 (the vertical dashed line), then the two groups (placebo and medication) are NOT statistically significant. If they do not touch 1, then they ARE statistically significant. Got it? To put it most simply, left of the dashed line is good, right of the line is bad.
So, the pediatric Odds Ratio does not include 1; this result supports the decision made in 2004 to add a black box warning that says these medications are associated with an increase in suicidal thoughts or behavior. (As it turns out, it is just thoughts, not behavior, but I'll address that in the second post.)
The 18-24 year-old Odds Ratio does include 1 (0.91-2.70), thus we cannot say that there is an increased risk.
The 31-64 year-old Odds Ratio just includes 1, but the estimated O.R. is less than 1, meaning that we cannot say there is a decreased risk, but there almost is.
For the over 65 group, there is clearly a significantly decreased risk of suicidal thoughts or behaviors. Note that these appear to be rare events... 12 people out of 3227 taking medication, and 24 out of 2397 taking placebo reported suicidal thoughts or behaviors. Hard to believe that only 1% of people with major depression had suicidal thoughts, huh?
Okay, so here is what the committee decided:
- There is a clear relationship between age and suicidal thoughts or behaviors in people taking antidepressants.
- Keep the black box warning that currently exists, but be very cautious about discouraging depression treatment and attempt to include balancing language that states that the risk of suicidal thoughts or behaviors when not taking medications should be considered. (They do not have data that tells them what that number is.)
- Encourage careful monitoring of all people being treated for depression.
- Extend language in the black box to indicate that the increased risk of suicidal thoughts or behaviors extends to around age 25, where it starts to drop off and become a decreased risk in the 30's and up.
- Encourage collection of data on the "activation syndrome" that some people get when taking antidepressant medications, especially SSRI's.
- Encourage collection of data which differentiates between suicidal thoughts and suicidal behaviors.
More later this evening.
