Dinah, ClinkShrink, & Roy produce Shrink Rap: a blog by Psychiatrists for Psychiatrists, interested bystanders are also welcome. A place to talk; no one has to listen.
Saturday, October 20, 2012
Kids and Mental Illness
I try to stay out of the whole Kiddy Bipolar Debate debate: none of the Shrink Rappers see children, so my knowledge of childhood psychiatric disorders is limited to what I saw during a 3 month inpatient rotation 20 years ago, what I read, and what I see of children in my personal life. It's a messy topic.
I brought it up today because the Wall Street Journal has an article that summarizes nicely all the issues, the issues with regard to diagnosis, the fear of over-treating, the problem with under-treating, the question of whether mood dysregulation in children should be a separate disorder. Please see Shirley Wang's article The Long Battle to Rethink Mental Illness in Children.
I'm glad they're leaning towards renaming bipolar disorder in children. When you hear Bipolar Disorder, you think about a lifelong condition that requires medication forever. Children have phases, behaviors occur in some arenas and not others. Perhaps if a child's emotional life is intolerable to them, or their behaviors make it impossible to function in their worlds, it's worth the risks to administer medications. But a kid throwing horrible tantrums, fighting, running around the room, does not necessarily evolve into the same category as an adult who has 3 episodes of depression, and 2 episodes of psychotic mania, during their lifetime. Oh, and I'm the one who thinks we should Rethink all of the Bipolar Diagnosis, not just for kids.
So Wang writes:
At one of his group's first in-person meetings, the NIMH's Dr. Leibenluft, an expert on bipolar disorder in children, gave a 20-minute PowerPoint presentation with evidence for a potential new disease. She called it Severe Mood Dysregulation.
She described a decade of studying children with severe mood problems that don't fit neatly into current illnesses. Thus began a cerebral process to decide what these kids might be suffering from.
The two main options: Create a new disease, or create a variant to an existing disorder. The discussions ran for years.
Wednesday, May 30, 2012
WhatsMyM3?
What’s your mental health number?This is the question that the Bipolar Collaborative is asking, using its WhatsMyM3 screening tool [PubMed]. “Many other illnesses have a 'number' that one can track – cholesterol, high blood pressure, diabetes. What’s the number for mental health?” asks Michael Byer, president of M3 Information, based in Bethesda, Md.~from Clinical Psychiatry News
Today's USA Today newspaper ran a story titled, "Screening for mental illness? Yes, there's an app for that," by Michelle Healy.
WhatsMyM3 is a validated, 3-minute tool that screens for symptoms of depression, bipolar disorder, PTSD, and anxiety, and can be used to monitor changes in symptom severity over time.
One of the developers, Michael Byer, approached me about a year ago for my opinions on development and use of the screening tool. Disclosure: After reviewing the research and seeing how useful it is, I have become more involved in the organization, becoming an adviser to the group that was started nearly ten years ago by past NIMH chief, Robert Post MD. (listen to podcast #63)
 It differs from other mental health screening tools, such as the PHQ-9 and the MDQ, in that these are all unidimensional -- they only measure one domain of symptoms. The M3 is multidimensional, measuring four areas of symptoms. Furthermore, when compared to results from the standardized interview tool, the Mini International Neuropsychiatric Interview (the MINI measures for 15 different mental illness diagnoses), WhatsMyM3 provides a total mental health score that is 83% sensitive in finding true positives and 76% specific in finding true negatives. In addition to the total score, there are four subscores, one each for depression, bipolar, PTSD, and anxiety.
It differs from other mental health screening tools, such as the PHQ-9 and the MDQ, in that these are all unidimensional -- they only measure one domain of symptoms. The M3 is multidimensional, measuring four areas of symptoms. Furthermore, when compared to results from the standardized interview tool, the Mini International Neuropsychiatric Interview (the MINI measures for 15 different mental illness diagnoses), WhatsMyM3 provides a total mental health score that is 83% sensitive in finding true positives and 76% specific in finding true negatives. In addition to the total score, there are four subscores, one each for depression, bipolar, PTSD, and anxiety.Put another way, the negative predictive value of the total score is 89%, meaning that if you score under the threshold, there is an 89% chance that you do not have any mental health diagnosis by the MINI. As with most screening tests, you want the negative predictive value to be high so that you don't have to subject the "negatives" to more specific testing. The positive predictive value, or PPV, is generally lower for screening tests. It is 65% for WhatsMyM3, meaning that if you score positive (total score >= 33 and positive for functional impairment), the odds of you having a diagnosis is almost two-thirds. A clinical evaluation can then help to determine if you do have a diagnosis. (Note: this tool cannot give you a diagnosis; it can only describe your relative risk of having, or not, a diagnosis.)
What people have found to be most helpful is using WhatsMyM3 to monitor their symptoms over time once they do have a diagnosis. This can be done for free on the website, or for $2.99 using the iPad or iPhone apps, or the Android app. For mental health clinicians, they can download the free M3Clinician iPad app and then screen their own patients. For about a dollar per screen, they can register their patients who want to track their symptoms over time and share their scores with the clinician. Primary care providers also purchase screens, and can even obtain insurance reimbursement by billing for an annual health risk assessment. The patient reports can be viewed by logging into m3clinician.com.
A sample report for a fake patient can be viewed here.
I think this sort of tool, or app, is exactly the sort of mHealth thing that empowers consumers to better manage and become engaged in their health care needs. This is happening in other areas, like diabetes, heart disease, and obesity. Mental health is also making great strides in mHealth.
 I should also point out here that the folks at M3 Information were the only ones to take us up on our offer of a free "advertisement" on Shrink Rap in return for donating at least $200 to our NAMIWalk for Mental Health Month (we don't typically accept display ads). A logo ad will be running soon on Shrink Rap soon for two weeks in recognition of their charitable donations. It will look like this and link to the iPhone and Droid apps. [We received no money ourselves from M3 nor from NAMI. We've never accepted any money from Pharma companies, nor does M3.]
I should also point out here that the folks at M3 Information were the only ones to take us up on our offer of a free "advertisement" on Shrink Rap in return for donating at least $200 to our NAMIWalk for Mental Health Month (we don't typically accept display ads). A logo ad will be running soon on Shrink Rap soon for two weeks in recognition of their charitable donations. It will look like this and link to the iPhone and Droid apps. [We received no money ourselves from M3 nor from NAMI. We've never accepted any money from Pharma companies, nor does M3.]Thursday, May 17, 2012
Conversations About Bipolar Disorder
If you wouldn't mind talking to her, do visit her site!
Wednesday, May 02, 2012
Blame the DSM?
About a year ago, a young mother called me, extremely distressed. She had become seriously sleep-deprived while working full-time and caring for her dying grandmother every night. When a crisis at her son’s day-care center forced her to scramble to find a new child-care arrangement, her heart started racing, prompting her to go to the emergency room.
After a quick assessment, the intake doctor declared that she had bipolar disorder, committed her to a psychiatric ward and started her on dangerous psychiatric medication. From my conversations with this woman, I’d say she was responding to severe exhaustion and alarm, not suffering from mental illness.
Caplan goes on to express her concerns with psychiatric diagnoses, the DSM, the problems with these labels that lead to the use of dangerous medications. Oh, we've been here on Shrink Rap before, see "Diagnostic Labels That Change Lives".
Caplan continues
In our increasingly psychiatrized world, the first course is often to classify anything but routine happiness as a mental disorder, assume it is based on a broken brain or a chemical imbalance, and prescribe drugs or hospitalization; even electroshock is still performed.
According to the psychiatrists’ bible, the Diagnostic and Statistical Manual of Mental Disorders (DSM), which defines the criteria for doling out psychiatric labels, a patient can fall into a bipolar category after having just one “manic” episode lasting a week or less. Given what this patient was dealing with, it is not surprising that she was talking quickly, had racing thoughts, was easily distracted and was intensely focused on certain goals (i.e. caring for her family) — thus meeting the requisite four of the eight criteria for a bipolar diagnosis.
When a social worker in the psychiatric ward advised the patient to go on permanent disability, concluding that her bipolar disorder would make it too hard to work, the patient did as the expert suggested. She also took a neuroleptic drug, Seroquel, that the doctor said would fix her mental illness.
Caplan goes on to say that because of the existence of a psychiatric label-- one she contends is wrong-- the patient lost her friends, her marriage, her home, her self-confidence, her wealth, was forced to move across the country to somewhere she was isolated, and the six weeks she spent on medication (presumably Seroquel) left her with a condition that may someday leave her blind.
Mental health professionals should use, and patients should insist on, what does work: not snap-judgment diagnoses, but instead listening to patients respectfully to understand their suffering — and help them find more natural ways of healing. Exercise, good nutrition, meditation and human connection are often more effective — and less risky — than drugs or electroshock.
Caplan, a Harvard psychologist, goes on to discuss a complaint she is helping to file against the DSM editors on behalf of 10 patients who were misdiagnosed. "Psychiatric diagnoses," she concludes, "are not scientific and they put people at risk."
-------------
Where do I even begin? Please, please, I don't know the patient, I only know the presentation given, and I'm going to be very sarcastic, because the way it was presented struck me a ridiculous and it distracted from some valid points that might have been made if there wasn't the Evil, Idiot Psychiatrist Theme with a sensationalist tone. Shame on the Washington Post for printing this.
Okay, so I couldn't quite follow the case she presented, at first it sounds like the patient went to the ER with symptoms of a cardiac problem, or exhaustion, or a maybe a panic attack. Perhaps, but some imbecile ER doc did a check list of symptoms, told her she had Bipolar disorder, and without even listening to her, weighing other options, or taking into consideration the context of her life, sent her off with Seroquel and a recommendation for therapy. This misdiagnosis then destroyed her life, because why would her husband and friends stick with her if she's got bipolar disorder? What better time to leave your wife then when her grandmother is dying, she's stressed out and sick? So she went to the ER because she was tired and her heart was racing. I think they see this all the time...I think they do an EKG and perhaps make sure the patient isn't having a heart attack or arrhythmia, and if they think it's anxiety, the patient gets a dose of a benzodiazepine, and gets sent home. Okay, but it's an ER and the docs are rushed and focused on what the patient needs now. They make wrong diagnoses all the time, and it's not just psychiatry, and it's not just because the doctor is sitting there with the DSM or has memorized the hundreds of possible diagnostic criteria.
Okay, but it turns out that she was on a psychiatric ward. You can't get admitted to a psychiatric ward because you're tired, with racing thoughts, a fast heartbeat, talking fast and being distracted. Pretty much, you need to be a danger--, suicidal, or having severe hallucinations or delusions, or be in extreme distress in some way. This was a wealthy patient who could afford outpatient care. All I'm sure of, is there is something more to the story.
Finally, the patient was admitted to a psychiatry unit, so presumably there was a second doctor who met with the patient and a treatment team that observed her behavior for a few days. Okay, I've stories of really lousy inpatient care, and I do believe the diagnosis could still be wrong and the treatment that was recommended might be wrong, or helpful at the moment but not necessary for the long-term, but I don't buy that a misdiagnosis let to the complete demise of this patient's life and a need to move across the country. These are the types of problems one sees as a result of the behaviors a person might have because they have a mental illness, perhaps one such as bipolar disorder.
So I don't know the patient, or the diagnosis. But I do know that the entire premise for this article is based on the idea that the patient was simply tired and stressed and perfectly normal and did not have a psychiatric disorder (the author tells us this) and this label alone destroyed her life. The reader is not allowed to even entertain the idea that the patient had a psychiatric disorder-- that maybe the psychiatrist did get some history and make reasonable observations, and the patient really did have bipolar disorder? (Obviously, I don't know this). There's no mention of a review of the records, discussion with family, interview of the doctor, Caplan is telling us her impression based on the patient's report only. Maybe the patient had panic disorder, or a personality disorder, or even an adjustment disorder (perfectly possible given the stresses involved). Oh, but then she took a bum recommendation to go on disability, and she got it! I've seen really sick people not get disability. It takes a lot of documentation and the government looks for ways to avoid paying this-- you don't get disability for having a psychiatric diagnosis, you have to be disabled by it. So, somehow, this patient who was simply exhausted and stressed, with No Psychiatric Disorder, per Dr. Caplan, managed to get admitted to a hospital and get disability benefits.
There were some valid points Caplan could have made. The DSM is not a 'scientific manual.' Personally, I don't find it terribly helpful in clinical practice. I don't keep a copy in my office (I bought one to use while writing Shrink Rap), and I'm not planning to buy the DSM-V. The overall concept is good, and it's very helpful to researchers to be certain that the groups they study have some diagnostic reliability, otherwise there is no way if knowing if a certain treatment addresses a specific group of people who can reliably be classified as having a specific illness. This isn't all bad, but I don't need 370-400 diagnosis for my work (predicted in the new DSM-V). And Caplan makes the statement that the editor, Allen Frances, says the work is based in science but has spread it's net too far. If you read Dr. Frances' blog, you'll note that he is quite skeptical and opposed to many of the proposed changes for DSM-V. It's not like the psychiatrists aren't thinking hard about these diagnostic categories and the ramifications they have. Still, I'm skeptical about how we think about these disorders, especially Bipolar Disorder.
I agree with Caplan that psychiatrists should listen more. Fifteen-minute med checks have made a mockery of our profession. I also tell all of my patients to exercise, eat healthy, and look for ways to solve their problems. But to imply that these things are the answers for the majority of people who are suffering (and often too distressed, depressed, and unmotivated, to just pull up their bootstraps, get up and exercise and cook a healthy meal )-- is an insult. You know, sometimes those things really do work, but if people are able to do those things, they've often tried them before seeking psychiatric opinions. To read Caplan's piece, you'd think everyone is an idiot. And finally, ECT: it still in use because some people find it helps.
Okay, I am ranted out.
Wednesday, October 19, 2011
Ups and Downs--The Bipolar Diagnosis
 I want to thank all of the people who commented on my post What is Bipolar Disorder. Your comments were tremendously helpful. The descriptions of what it feels like to have this illness were incredible-- vivid, heartfelt, almost a mix of poetry and misery-- the stories were told in a way that I don't often hear in clinical settings. So, thank you. And if you're someone who doesn't read the comment section of blogs, I would urge you to make an exception for this post. The comments speak to what an intelligent, educated, and articulate readership we are lucky enough to have join us here, and the commenters make the experience of difficult mood states come alive in a way it is so hard to do with words. A little bickering (it wouldn't be Shrink Rap without that!), but I want to point out that the issues that inspired the bickering are exactly the concerns we address in figuring out the usefulness of the expanded bipolar diagnosis.
I want to thank all of the people who commented on my post What is Bipolar Disorder. Your comments were tremendously helpful. The descriptions of what it feels like to have this illness were incredible-- vivid, heartfelt, almost a mix of poetry and misery-- the stories were told in a way that I don't often hear in clinical settings. So, thank you. And if you're someone who doesn't read the comment section of blogs, I would urge you to make an exception for this post. The comments speak to what an intelligent, educated, and articulate readership we are lucky enough to have join us here, and the commenters make the experience of difficult mood states come alive in a way it is so hard to do with words. A little bickering (it wouldn't be Shrink Rap without that!), but I want to point out that the issues that inspired the bickering are exactly the concerns we address in figuring out the usefulness of the expanded bipolar diagnosis.That said, I wrote my article for Clinical Psychiatry News, called Rethinking Bipolarity. If you click the link at the end, it will cycle you back to the What is Bipolar post. Let me know how I did?
And thank you, again. Thank you also to Dr. Dean MacKinnon, of the Johns Hopkins Mood Disorders Center and author of Trouble in Mind for previewing the article for me.
Sunday, October 16, 2011
What is Bipolar Disorder?
Also, please just off the top of your head, I can read DSM or Google myself, and I'm more interested in your ideas about what exactly the disorder is.
I may not use your responses (I sort of know what I want to say) but no matter what, I'm curious.
Thank you so much...
Friday, August 05, 2011
Retriever Blog: Fad Diagnoses in Kiddie Psychiatry?
In response to Joy Bliss' post (Fad diagnosis in Psychiatry: Bipolar Disorder in children) on Maggie's Farm, Retriever wrote about her experience with a child with an early and severe mental illness, and short-sighted attempts to reduce access to needed intensive mental health treatment for children.
I do think that diagnosing behavior problems in kids has been overextended, due more to loose interpretation of current diagnostic criteria rather than to overbroad criteria. But let's not throw the baby out with the bath water.
(Speaking of water, taking a break here from vacation to post an image from Southwest Harbor, Maine.)
Monday, October 04, 2010
I Have Bipolar Disorder. Can I be a Doctor?

Ah, one of our readers asked this.
It's one of those questions to which there is no real answer. Being a doctor takes a long time, it requires reliability, diligence, and a willingness to learn things you may not want to learn (organic chem anyone????) and do things you may not want to do. It requires endurance and passion. You need to be tolerant of many things: arrogant supervisors, irritable colleagues, sick people who may not be charming and who may, in their distress, be down-right nasty. You have to tolerate a militaristic order and be willing to work with a system that may be very difficult, wrong, and demand your obedience in ways that may be uncomfortable. Oh, I am so happy to no longer be a medical student or a resident in training.
So can you do it with bipolar disorder? Can you do it with diabetes? Can you do it with attention deficit problems? Can you do it if you're disorganized or ugly?
The question assumes there is one bipolar disorder, that for everyone it has the same course and the same prognosis. Some people have an episode a few times in a life, and between episodes, their mood is stable, their emotions gentle. Others cycle from one mood to another, feeling the whole bipolar thing most minutes of most days. Some patients with bipolar disorder are in and out of the hospital, behave in impulsive and criminal ways when ill, and can't hold any job. Some do fine with medications and therapy, while others have refractory conditions that defy the most creative of cocktails and the best of therapists, even with their total compliance. And some people become doctors and then get bipolar disorder.
So, maybe.
What do we think Kay Jamison would say?
Sunday, September 19, 2010
Brilliant Versus Crazy, Revisited.
In today's New York Times in "Just Manic Enough-- Seeking Perfect Entrepeneurs," David Segal writes about enterpreneur Seth Priebatsch:

According to the Diagnostic and Statistical Manual — the occupation’s bible of mental disorders — these symptoms include grandiosity, an elevated and expansive mood, racing thoughts and little need for sleep.
“Elevated” hardly describes this guy. To keep the pace of his thoughts and conversation at manageable levels, he runs on a track every morning until he literally collapses. He can work 96 hours in a row. He plans to live in his office, crashing in a sleeping bag. He describes anything that distracts him and his future colleagues, even for minutes, as “evil.”
He is 21 years old.
So, what do you give this guy — a big check or the phone number of a really good shrink? If he is Seth Priebatsch and you are Highland Capital Partners, a venture capital firm in Lexington, Mass., the answer is a big check.
But this thought exercise hints at a truth: a thin line separates the temperament of a promising entrepreneur from a person who could use, as they say in psychiatry, a little help. Academics and hiring consultants say that many successful entrepreneurs have qualities and quirks that, if poured into their psyches in greater ratios, would qualify as full-on mental illness.
------------
There are people who are bright, exuberant, fast-thinking, productive, and filled with energy and ideas. It's a question we've been asking for a while: is this a temperament or a disorder? I would contend that no one goes to a psychiatrist saying "Hey, I accomplish too much, I'm happy and have a lot of energy." People come to psychiatrists because they are suffering, or because they've moved far enough from reality that others are alarmed. We can joke an call it 'hypo-mania' but it's where we'd all like to be.
Having said that, it feels like Segal writes this from the perspective that his subject is certainly not ill. Psychiatric diagnoses are made over time and it seems perhaps irresponsible to use high-energy, successful people as examples of those who might be teetering on some genius--insanity tightrope. The answer ---if there is one-- lies in the course of a lifetime. If the same highly productive, sleep-defying entrepreneurs later become depressed, despondent, and unable to crawl out from under the covers, then it would certainly make sense to consider periods where he went 96-hours without sleep as part of the whole picture. If such a person never becomes depressed, well....they make lots of money, stay far away from shrinks, and oh, can I have a little of that energy?
Thanks to Jesse for telling me about the article. My New York Times didn't come today. You'd think with all the free publicity I give them on Shrink Rap.....
Wednesday, August 25, 2010
Emotion versus Mental Illness

My favorite commenter, "Anonymous," wrote in to my Duckiness post to say that it was good I could post something totally silly without being told I need more meds. Oh, if life were that simple. And it is true that once someone has a diagnosis of bipolar disorder, not only does the world question their emotions in a black & white "are you sick again?" kind of way, but patients don't trust themselves to feel for it's own sake.
If you're not sick, then being asked if you took your meds is insulting and degrading. And so I thought I'd put together some guidelines for Emotion versus Mental Illness. I'm inventing this as I go, with no evidence-based anything, so take my suggestions at your own risk.
- If you are ultra-successful, rich, brilliant, gorgeous, famous, and comfortable with your diagnosis, you may want to consider telling people you have a mental illness because it decreases stigma and people like being with the ultra-successful rich, famous, brilliant and gorgeous and won't care that you have a mental disorder. It helps even more if you're charming.
- If you're not ultra-successful, you may want to pick and choose who you tell that you've been ill and are on medications. This isn't always possible, especially if your illness is evident to others or if the presentation of your symptoms resulted in a hospitalization. It's good to tell close family members.
- If multiple people are looking at you strangely, or commenting on your behavior, or saying you need medications, you might want to at least entertain the option that you could be sick. Unfortunately, poor insight and judgment are symptoms of mania.
- Tell the people close to you not to make medication jokes. It confuses the issue if you seriously do need medication changes, and it's rude, degrading, dismissive, and disrespectful. There, I said it.
- If you want to be silly, go for it. Be silly when you're well so that being silly is part of your baseline personality and no one equates this with being out-of-character. You'll note the duck invaders did not come after me, rather they said, "There's Dinah posting yet another stupid duck post." If I'd posted about why chocolate should be outlawed and made into a controlled substance, those same duck invaders would be asking "What's wrong with Dinah?"
- Mental illnesses come as constellations of symptoms. There is no "Sending out silly duck stuff" as a symptom. People think about mania when the ducks are combined with more energy, racing thoughts, a decreased need for sleep, increased mood OR irritability, and other symptoms of mania. Know the list and if someone bothers you, say, "I posted about ducks, I do not have any other associated symptoms." Recite them if necessary. If you do have the other symptoms, refrain from posting about ducks. I don't want Posts Duck Blog Posts to show up anywhere in DSM-V and these days you just never know.
- No one controls how any other person thinks of them or judges them and it's not reasonable to live life ruled by a desire to be perceived in a certain way . It's another form of poultry, but Don't Let the Turkeys Get You Down. There are a lot of turkeys out there.
Moods happen on a spectrum. Some people have large variations in their mood---large enough or severe enough such that it causes suffering, and we call it an illness. Some people don't have much variety to their moods and live in a calm, even-keel place, and it's great that we have such people. But, I absolutely promise you that if we lived in a world where everyone had a very narrow range of mood, this would be one terribly boring planet. We should celebrate our diversity, not condemn those who like ducky stuff.
Friday, October 23, 2009
Only Perfect People Should Have Children

I hope you know that the title of this post is sarcastic.
A reader wrote to us and asked if we'd address the issue of whether people with bipolar disorder should have children:
"I have been asked how I could have had children knowing I had bipolar and the person asking would never have known I had bipolar if i did not told them."
I enjoyed thinking about this, but I'm punting. I really don't like the idea of putting a value judgment on who should or shouldn't have children. Truly, there are a lot of people out there who shouldn't have babies (because they can't take care of them), but do, and a lot of wonderful people who've been born to people who maybe shouldn't have had babies, but did, and we're all glad they got born anyway. There are no guarantees in life, and I've never heard anyone put out a blanket statement that people with psychiatric disorders shouldn't have children.
Thoughts?
Thursday, September 18, 2008
Mood Disorders 101

In yesterday's post, I talked about how Ron Pies questioned the difference between depression and "proper sorrows of the soul"-- ah, Dr. Pies was quoting some dead monk-- and Lily mentioned that she was just diagnosed with Bipolar II. It got me thinking that we should say something about how a psychiatrist thinks about mood disorders. If you're a psychiatrist, you can go home now, today's blog post is not for you.
I'm going to start by saying that I'm typing this off the top of my head, I'm purposely not pulling out the DSM (Diagnostic Statistical Manual), I'm just rambling. I'm very good at rambling. So this is how I think about mood disorders and how I go about reaching a diagnosis.
In the course of the day, a person without a mood disorder generally feels "fine." People go through life with a fairly steady mood, not too good, not too bad. Sure, stuff effects mood, and it may vary some-- people feel transiently ecstatic about wonderful things happening, people feel sad about distressing things happen, and there's the unexplained 'bad hair day' also known as 'waking up on the wrong side of the bed.' Let's take it as a given that people have moods, they vary some, sometimes the reason is obvious, and they aren't generally extreme.
Mood itself is a good place to start. Mood variation alone is not enough to make a diagnosis of a mood disorder (weird, huh?) and someone who feels very sad, even a lot, who has no other symptoms of depression, isn't called depressed. So someone is trekking along just fine and then suddenly they start feeling down/sad/miserable and at the same time other symptoms emerge. These symptoms may include: changes in sleep, appetite, a decrease in the ability to feel pleasure, loss of energy, loss of interest, decreased sex drive, irritability, guilt, a feeling of being physically unwell, hopelessness, helplessness, thoughts that death might be welcome, or thoughts of suicide. People who have pain syndromes will have worse pain, people with Parkinson's Disease may have worsening of their movement disorder, people with dementia may have more trouble with their memories, food may seem tasteless, colors may look less bright. People's thoughts change-- these are the cognitive symptoms of depression-- with a tendency to see oneself in negative ways, to take on blame, to block or discount all positive feedback the world might give. You can't have just one symptom to be diagnosed with Major Depression, you have to have a few symptoms and they have to occur together, because mood disorders are 'syndromic' illnesses: they are defined by the co-occurring constellation of symptoms. The same person may have different symptoms during different episodes of depression, but generally episodes are discrete, and with or without treatment, they usually abate eventually.
There are some people who don't see their depressions as discrete episodes but feel they've been depressed for a very long time. Maybe they have Major Depression, but there is also a condition known as Dysthymia which is a chronic, low grade depression which lasts for years (--at least part of the day, most days, for at least 2 years, I think). This version of depression is not as striking as an episode of Major Depression-- the symptoms aren't as severe, abrupt, or debilitating and other people are often not as tuned in to the sufferer's distress.
That's the down side of mood.
Then there's the Up side of mood. Mania is the extreme up state, and the associated mood state is either elated/ecstatic or extremely irritable. Again, a simple shift in mood is not enough to diagnose an illness, there need to be some associated symptoms which occur at the same time as the mood elevation/extreme irritability. Manias include an increase in energy and a decrease in the need for sleep. The issue of Need for Sleep is important here: it's not normal to be awake and active for days at a time and not feel tired, this is much different than insomnia. People may have more ideas, they may have completely irrational ideas, judgment becomes impaired, thoughts may flow much faster, sometimes racing so fast that the patient can't keep up with them. Activity increases, speech may become fast and pressured. The person may feel very very good about themselves, very optimistic and positive, or believe they have special powers. There may be an increased interest in sex or religion, and people may spend lots of money on things they wouldn't normally spend on. Behavior may become impulsive and insight is often very impaired. The manic patient often resists the idea that they have an illness, and doesn't see how outrageous their behavior has become. They may hallucinate (see or hear or feel things that aren't there) or have delusions, particularly of grandeur, but sometimes of paranoia. Full blown mania is not subtle and often results in psychiatric hospitalization.
Anyone who has had even a single episode of Mania, ever, is diagnosed as having Bipolar Disorder, Type I, what used to be called Manic Depressive disorder. Do note that a person can be diagnoses as having Bipolar Disorder even if they've never (or Not Yet) had an episode of Major Depression. The fact is that it's extremely rare for someone to suffer an episode of mania and then live out life without ever having an episode of depression, that manias tend to recur (sometime after decades) and that it's not unusual for a person to have an episode of mania and then 'crash' into an episode of depression. Anti-depressants and steroids can precipitate an episode of mania and we still don't know if those manias have the same implication for lifelong diagnosis.
So mania isn't subtle, but there are people who have episodes of elevated mood states without the extreme symptoms. Maybe they have periods of time where their mood is better than the norm of fine/okay/good, and their energy is increased, and they are more productive or impulsive, and revved up than the usual even-keel. They may look good, feel good, live life a little more grandly. This may be subtle, and it's this state of elevation that is called Hypomania. This mood state may be hard to differentiate from a high-energy person, an anxious person, someone with Attention Deficit Disorder, or just the way that everyone wishes they could feel all the time. Hypomanias do not result in psychiatric hospitalizations and are not accompanied by extremes in behavior, hallucinations, or flagrant delusions. Hypomanias alone do not generally result in someone coming to psychiatric attention and patients present during episodes of Depression. This is Bipolar Disorder, Type II.
People with Bipolar Disorder, type II, generally spend much more time depressed than hypomanic, their depressions may be harder to stablize, and they often do better if a mood stabilizer is added to the treatment regimen.
If this isn't all confusing enough, there is a diagnosis called Cyclothymia, which means that a person's moods vary from hypomanic to mildly depressed, but none of the episodes of depression is severe enough to warrant a diagnosis of Major Depression. Psychiatrists don't use this diagnosis very much.
Okay, I'm going to add one more thought and then I'll shut up. Borderline Personality Disorder is a condition that includes "affective (=mood) instability" and the differentiation between a personality disorder and a mood disorder can be difficult even for experienced psychiatrists.
Wednesday, September 17, 2008
Psychiatry Stuff in the New York Times.

Should I give him a diagnosis of clinical depression? Or is my patient merely experiencing what the 14th-century monk Thomas à Kempis called “the proper sorrows of the soul”? The answer is more complicated than some critics of psychiatric diagnosis think.
Saturday, June 28, 2008
True Emotions

Sunday, April 13, 2008
My Three Shrinks Podcast 45: Guest Ray DePaulo on Treatment Resistant Depression
We are pleased AGAIN to have the head of Johns Hopkins Psychiatry, Dr. J. Raymond DePaulo, joining us here to talk this week about treatment resistant depression (TRD), bipolar disorder, favorite quotes, and words we don't like.
Dr. DePaulo joined us on the last podcast (#44) and talked about cosmetic psychopharmacology, among other things.
April 13, 2008: #45 Guest Dr. Ray DePaulo on Treatment-Resistant Depression
Topics include:
- Treatment-Resistant Depression. How is it defined (~10:00 min into the podcast)? Is there a magic bullet? Treatment strategies (don't give up; remember lithium; use proven agents; get 2nd and 3rd opinions; do psychotherapy).
- Nellie, the Hypothetical Patient. Let her know what we know about treatment, and what we don't.
- "Alternative" Treatments. St. John's wort; SAMe (s-adenosylmethionine); omega-3 fatty acids; ketamine; vagal nerve stimulation (VNS); deep brain stimulation (DBS); psychosurgery (cingulotomy).
- Cognitive Therapy. Many different types.
- Words which are Unliked by the Podcasters. Alternative treatment. Mood stabilizer. Antidepressant. Antipsychotic. Hallucinogen. Psychosis. Neurosis. Organic. Schizophrenia. Nervous breakdown. Mood Swings.
- Quotations We Like.
"There's only two types of music: good music and bad music." Fran Liebowitz
"Eighty percent of success is showing up." Woody Allen
"Expect more of yourself and less of others; you'll be disappointed less." Unknown
"Life is unfair; the sooner you figure that out, the happier you will be." Unknown (Lilya said it in 2003 on a recovery forum)
"A good clinician is someone who makes prudent decisions based on insufficient information." Ray DePaulo (I think)
"Experience is what we call it when we were looking for something else." Federico Fellini
"Good decisions are based on experience. Experience is based on bad decisions." probably Mark Twain
"'Experience' is simply the name we give our mistakes." Oscar Wilde
"Science is a process of conjecturing and refuting what is thought to be universal, therefore a theory can only be considered 'scientific' if it is falsifiable," paraphrasing Karl Popper.
"It's a short step from the penthouse to the outhouse." Unknown (many found)
"It's a short step from Who's Who to Who's He." Unknown
"There ain't no such thing as a free lunch," or TANSTAAFL, by Robert A. Heinlein.
"When Momma ain't happy, no one's happy." Apparently, an old southern saying.
"For every aphorism, there is an opposite aphorism that's equally true." Unknown
"Children can be happy when their parents are miserable. But a parent is never happier than her unhappiest child." Laura Lippman
"Data is not knowledge, and knowledge is certainly not wisdom." Unknown
- Drugs in the Drinking Water. Brief mention of last month's AP story finding all sorts of pharmaceuticals in numerous municipal water supplies.
- Books we are reading.
-Ray: "Saint Augustine", by Garry Wills.
-Roy: "Valis", by Philip K. Dick. (Ben was reading it on "Lost".)
-Clink: More listening to an opera about Carmen, a famous female sociopath.
-Dinah: "How Doctors Think", by Jerome Groopman.

There are three audiences for this authoritative book: people who think they may be depressed, those whose condition has already been diagnosed and are in treatment, and those who are concerned about someone who is either in treatment or probably needs to be.
| Find show notes with links at: http://mythreeshrinks.com/. The address to send us your Q&A's is there, as well (mythreeshrinksATgmailDOTcom). This podcast is available on iTunes (feel free to post a review) or as an RSS feed. You can also listen to or download the .mp3 or the MPEG-4 file from mythreeshrinks.com. Thank you for listening. |
Monday, October 22, 2007
And Now a Word or Two about Mood Stabilizers

I came to talk about mood stabilizers and figured I'd start by summarizing our sidebar poll "What is Your Favorite Mood Stabilizer?" Only every time I come on, the poll has gotten more votes, so I guess I'm waiting for the mood stabilizer poll to stabilize.
Here's where we're at so far:
What's Your Favorite Mood Stabilizer?
Lithium | 32 (22%) |
Depakote (Valproate) | 27 (19%) |
Zyprexa (Olanzapine)/ other atypical anti-psychotics | 29 (20%) |
Carbamazepine (Tegretol) | 1 (0%) |
Gabapentin (Neurontin) | 9 (6%) |
Lamotrigine (Lamictal) | 44 (30%) |
143 votes, Lamictal has been consistently in the lead since the beginning. Both surprising and not surprising.
I talked about How A Shrink Chooses an Antidepressant. I have less to say about how a Shrink Chooses a Mood Stabilizer. In fact, I'm not really sure. I'll tell you how This shrink chooses a mood stabilizer. It's not that much different, so click on the that post for more details.
- History of Past Response.
- Family History of Response
- Patient Preference. This is a big one with mood stabilizers. The gold standard is Lithium and some patients just won't hear of it. They think taking lithium means they're really far gone, that it's heavy duty stuff, that it means they're crazy.
- Medical issues: lots of them with mood stabilizers.... lithium can effect the thyroid and kidneys, it interacts with lots of other meds, depakote can effect the liver, so can tegretol, lots to think about, lots to monitor.
- How strongly I'm convinced that the patient has had a full blown manic episode. Plenty of people say "I'm Bipolar" but the history doesn't reveal a story for episodic, syndromic co-occurance of the hallmark symptoms of mania: elevation in mood or irritability, increased energy/ decreased need for sleep, quickening of thoughts or speech, impulsivity with regard to spending, sexuality, religion, hallucinations, grandiose delusions, inflated sense of worth or well-being. None of these symptoms alone are enough to diagnose mania, ya gotta have a few and they have to occur at the same time as the other symptoms. Lots of people shop impulsively to cheer themselves up, lots of people have periods where they feel more energetic and productive, lots of people get happy when they win the lottery. It's sometimes hard to get a history for a syndromic diversion from a baseline (or pre-morbid) personality.
- If I think someone definitely has bipolar disorder, and there isn't a reason not to use it, I start with Lithium. It's a good mood stabilizer. It's cheap. I'm familiar with how to use it. It's also a good anti-depressant augmenter. Despite all the hype about the awful side effects (weight gain, nausea, tremor, cognitive slowing, renal and thyroid impairment), I've seen lots of people have good responses and not have any side effects, so I start with that assumption and I use low doses. If the patient gets better, I don't push the level, even if it's really low. If the patient has intolerable side effects, I try another preparation of lithium (eskalith, lithobid), and if that doesn't work, I stop it and try another med. Why do I like lithium? I think because I've heard enough people put up resistance, then try it and come in saying "I feel normal for the first time." The down side is that you have to do bloodwork every 3-4 months even if the patient is well and has no symptoms.
- If I'm not so sure about the manic component as a real, syndromic entity, and the primary complaint is depression, I start with Lamictal. The upside-- it's well tolerated, people like it, there's no routine labwork and there's no stigma. The down side-- slow going to build up from a dose of 25mg to the therapeutic range of around 400mg. Another down side-- that fatal rash risk. And the final down side-- I've heard a couple of anecdotes of patients who have ended up in the ICU with rashes, liver zorkout, life-threatening problems. Not a lot, but it only takes one such story to make you hold your breath when you write a prescription and I have a friend who says "I'll never be able to prescribe Lamictal again." It's not science. I actually tell patients this story-from-hell when I prescribe it, and they'll still take it over lithium. Mostly, it's a good medication, it's well tolerated, and it helps.
- If a patient doesn't want Lithium, I prescribe depakote. It's associates with it's own issues, including weight gain, needs lab monitoring, and if the patient doesn't have insurance, it's expensive and hard to get samples of.
- I haven't prescribed tegretol in ages and I wondered if the reason it's so unpopular on our sidebar is because it isn't used so much.
- I prescribe anti-psychotic medications to people who are agitated, acutely suffering, not sleeping, in need of something quicker than lithium/depakote/ or lamictal. These medications work, they're well-tolerated, patients like them. And I worry about the metabolic effects and wish there was some free ride.
- Sometimes I use one of the older anti-psychotic-- navane may be my favorite
- If there is no history of substance abuse (---hmmm, that's rare in people with bipolar disorder), I may prescribe some ativan or klonopin for the short term.
- I haven't used Trileptal, I don't know why. I have a patient or two on Neurontin, I stopped prescribing it when studies showed it didn't help with mood stabilization. Perhaps I was wrong. And I haven't seen very many people tolerate Topamax, though I have seen it work wonders for migraines.
- Lithium is my favorite.
And to one of our anonymous commenters who wrote in:
Tuesday, April 17, 2007
My Three Shrinks Podcast 16: Encyclopedia of the Weird

ClinkShrink here. I volunteered to help Roy by editing one of our podcasts--heaven help me, I did the best I could. Be patient, I'm using Windows. This is podcast number 16 which was actually podcast number 14 taped about a month ago and taken out of order for no particular reason.
April 17, 2007
Topics include:
- First up are the Top 25 Crimes of the Century, a topic that could only be mine. It's a Time article that lists some of the most infamous or unusual crimes, but I have a couple bones to pick about their choices. Roy and Dinah just think I'm weird for even knowing this stuff. [Listen in to find out Clink's favorite crime. -Roy]
- Next we answer a question from Driving Miss Molly regarding how much and what kind of preparations psychiatrists do before their patients' appointments.
- Finally we do the Shrink Rap blog rollcall, where Shiny Happy Person deals with medical training in the UK and under the NHS, Roy flirts with the Girl with the Blue Steth, and Intueri talks about bipolar disorder in kids.
Thank you for listening.
Saturday, June 10, 2006
Exercise Your Imagination
Given the recent post on atypical antipsychotics in children, I started thinking about our national epidemic of obesity. According to the CDC, here are the top ten states with the highest obesity rates, expressed in percent:
| Mississippi | 25.9 |
| West Virginia | 24.6 |
| Michigan | 24.4 |
| Kentucky | 24.2 |
| Indiana | 24.0 |
| Texas | 23.8 |
| Alabama | 23.4 |
| Louisiana | 23.3 |
| Tennessee | 22.6 |
| Missouri | 22.5 |
Presently 16% of children and adolescents in the United States are overweight. In addition to the commonly known medical complications of obesity, overweight children have significant psychiatric sequelae: peer and teacher stigmatization, depression, and social withdrawal. If the condition persists to adolescence, weight problems can precipitate eating disorders such as anorexia nervosa or bulimia. While treatment stategies exist, the prognosis is worsened if the condition begins in childhood and the child has at least one obese parent.
So far the evaluation of obesity in children has centered on identification of endogenous (medical) or genetic causes. Given that some atypical antipsychotics have been associated with substantial weight gain in children, drug-induced causes must also be considered.
Of course, all of these risks must be weighed (pardon the pun) against the morbidity and mortality associated with untreated bipolar disorder.
...ironically, in prisoners weight gain is considered a good thing---a healthy sign of returning nutrition after months of drug and alcohol abuse, or an indication that weight-training is paying off.
DOH...almost made it.
Friday, June 09, 2006
AGP: Antipsychotic use in kids increases
The New York Times highlights this week's article in the Archives of General Psychiatry
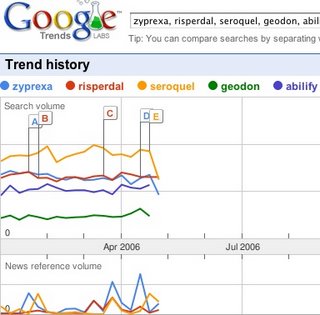
suggesting that the use of atypical antipsychotics in children continues to climb. At the top, you can see the relative rates at which folks enter 5 commonly-prescribed antipsychotics in Google's search engine. I would have thought that Zyprexa would have been #1 search, as it is the #1 cost drug for many state Medicaid formularies.
Nearly one-fifth of visits to psychiatrists included prescriptions for antipsychotics. This is quite disturbing, especially because nearly 40% of the kids are taking these for "disruptive behavior disorders". The drugs are approved for schizophrenia and bipolar disorders.
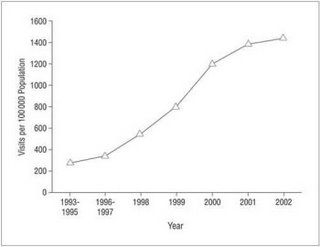
National trends in office-based visits by children and adolescents that included antipsychotic treatment, 1993–2002. Annualized visit rates per 100 000 population aged 0 to 20 years were calculated using National Ambulatory Medical Care Survey and US Census Bureau data:
from the NYT:
Dr. DelBello said that the field "desperately needs more research" to clarify the effects of the antipsychotic drugs, but that many children struggling with bipolar disorder get more symptom relief on these drugs than on others, allowing psychiatrists to cut down on the overall number of medications a child is taking.
Sunday, May 28, 2006
Roy Unleashed!

I checked the blog yesterday was surprised to find three, count 'em, three new posts by Roy! Is he manic, I wondered? Oh, probably not...just unleashing his pent-up blogs which have been festering... I can only speculate. But this brings me to an interesting study I found, one that pertains to Roy's comments on most frequent diagnoses among psychiatric patients. A landmark 1998 study by Sille, et. al. revealed that the most common psychiatric diagnosis among bloggers is, in fact, Bipolar Disorder, accounting for 61.8% of all psychiatric diagnoses (most recent episode being a Mixed State), followed by Obsessive Compulsive Disorder, with compulsive writing being the most common symptom, followed by compulsive email checking. In a follow-up study done by Monke in 2001, it was found in a randomized, placebo-controlled, double blind study that manic bloggers were more likely to report remission of symptoms, a return to euthymia, and a decrease in compulsive blogging, when treated with a combination of Depakote, chocolate and caffeine. Interestingly enough, none of the bloggers studied responded to either Lithium or any of the novel anti-psychotic agents.
Okay, so I made it all up, but I had fun doing it!





I hope you have a really great reason for purposely for gathering useless data.