Dinah, ClinkShrink, & Roy produce Shrink Rap: a blog by Psychiatrists for Psychiatrists, interested bystanders are also welcome. A place to talk; no one has to listen.
Friday, December 28, 2012
Monday, December 24, 2012
Check My Math
The APA put out a statement in response to the NRA's recommendation to put armed guards in every school. Quoting from the statement:
Only 4-5% of crimes are committed by mentally ill people because most violence is due to personality disorders combined with substance abuse, and once you combine that trifecta the number of people at risk of committing violence drops quite a bit.
Here are the prevalence rates:
ASPD 15% prevalence (per ECA study)
MI 25% prevalence
SA 10% prevalence (per NIDA)
The population of the US at this minute is 314,996,054 (US Census Bureau). So, at any point in time now we've got:
In other words, very few mentally ill people commit violence crimes because most of them don't have the main necessary risk factors. And there are relatively few people with ASPD running around so that when you throw in the MI folks it doesn't increase the pool that much. And when it comes to violent crime, a disproportionately small number of people commit the majority of offenses. The relative risk of a small number of violent offenders outweighs the small number of mentally ill people who have the trifecta. Does that make sense?
Ugh, I just spent far too much time trying to get the table formatting right and then Blogger messed up my HTML code. I give up. And I can't believe I'm writing about this the day before Christmas.
Happy Holidays!
Oh yeah, one more thing:
The APA response dings the NRA for conflating mental illness with "evil," and criticizes the NRA for using the term "lunatic." I'm going to ding the APA for referring to my prison patients as "evil." I'm going to object to that, big time. The people I treat may have poor judgement, may have substance abuse problems, may have done awful things during desparate times, but I have met very few truly evil people even in prison. Demonizing and dehumanizing criminals is a very very bad idea. These people are part of our society, they will be coming back to our cities and neighborhoods some day, and it does nobody any good to say that my correctional patients are evil people. Please.
“Only four to five percent of violent crimes are committed by people with mental illness,” said the APA’s president, Dilip Jeste, M.D. “About one quarter of all Americans have a mental disorder in any given year, and only a very small percentage of them will ever commit violent crimes,” he added.So Dinah sent me an email asking this question:
"So if 1/4 of all people have a mental illness in any given year, and 56% of people have a lifetime incidence, then why are only 4-5% of violent crimes committed by people with mental illnesses? It might seem that we'd all want to be mentally ill so we wouldn't be violent."My answer to that is:
Only 4-5% of crimes are committed by mentally ill people because most violence is due to personality disorders combined with substance abuse, and once you combine that trifecta the number of people at risk of committing violence drops quite a bit.
Here are the prevalence rates:
ASPD 15% prevalence (per ECA study)
MI 25% prevalence
SA 10% prevalence (per NIDA)
The population of the US at this minute is 314,996,054 (US Census Bureau). So, at any point in time now we've got:
| (per million) | ||
| MI alone | 79 | 314,996,054 x .25 |
| MI + ASPD + SA | 5.9 | 314,996,054 x .25 x .15 x .1 |
| ASPD + SA alone | 4.7 | 314,996,054 x .15 x .1 |
In other words, very few mentally ill people commit violence crimes because most of them don't have the main necessary risk factors. And there are relatively few people with ASPD running around so that when you throw in the MI folks it doesn't increase the pool that much. And when it comes to violent crime, a disproportionately small number of people commit the majority of offenses. The relative risk of a small number of violent offenders outweighs the small number of mentally ill people who have the trifecta. Does that make sense?
Ugh, I just spent far too much time trying to get the table formatting right and then Blogger messed up my HTML code. I give up. And I can't believe I'm writing about this the day before Christmas.
Happy Holidays!
Oh yeah, one more thing:
The APA response dings the NRA for conflating mental illness with "evil," and criticizes the NRA for using the term "lunatic." I'm going to ding the APA for referring to my prison patients as "evil." I'm going to object to that, big time. The people I treat may have poor judgement, may have substance abuse problems, may have done awful things during desparate times, but I have met very few truly evil people even in prison. Demonizing and dehumanizing criminals is a very very bad idea. These people are part of our society, they will be coming back to our cities and neighborhoods some day, and it does nobody any good to say that my correctional patients are evil people. Please.
Sunday, December 23, 2012
Happy Holidays! And Free Novels
Happy Holidays!
For the next 5 days, my three novels will be available as a free download to Kindle.
Double Billing is the story of a woman whose life changes when she discovers she has an identical twin she never knew existed. It's a short book and is intended to be a quick read. So I think it's my best shot at fiction.
Home Inspection is a story told through psychotherapy sessions in a format that is similar to the HBO series In Treatment. Dr. Julius Strand is a psychiatrist who plods along in his already-lived life until two of his patients inspire him through their own struggles to find love.
Mitch & Wendy : Lost in Adventure Land is about two siblings who are struggling with their relationships in the aftermath of their parents' divorce. The story takes place on Wendy's 10th birthday when the kids get lost in an amusement park, only to learn they are being followed by a man who knows all about them from Mitch's misguided Facebook life. Written for 4-5th graders, or the very young at heart.
If you don't own a Kindle reader, you can install a free Kindle app on your computer, tablet, or cell phone by going here and then you can read any Kindle book.
All three novels are also available as as paperbacks from Amazon.
Rather than giving different links to all these books and formats, there is a single link to my Amazon page with all the options here.
I'm more than happy to have people download my novels at no cost -- I'll be keeping the doctor day gig -- so please tell/tweet/blog/share the free promotions to anyone you think might be interested.
Finally, If you do read any of the books, please consider putting a review on Amazon.
Thank you so much and enjoy the season.
Dinah
The Accessible Psychiatry Project
Saturday, December 22, 2012
Letting Go
I don't think of myself as a workaholic, but there are moments in time where I find that my brain gets really stuck on work. Maybe there's a patient I'm worried about, or I'm working on an article that requires some searching, or is about something I'm passionate about. Ideas for blog posts run through my head, or every conversation somehow turns to CPT codes (~Yes, yes, this is my fault, Clink. Poor Clink has heard so much about CPT codes) or the latest issue of the moment. Or I get annoyed that the world makes no sense. I find that I stress myself out with things I really don't need to be stressed about, and then I really start to long for vacation. When I get in these states, I feel like the unfortunate thing about going on vacation is that I really need a vacation from myself! The good thing is that when I get away from work, the phone, the internet, the office, the house, the iPhone, the computer, --after a few days, I start to relax and eventually to recharge. There's something about our all-too-connected world that isn't always good for me, and I have this love-hate relationship with technology.
Okay, so today was my first day of vacation. I baked cookies, watched TV, cooked a gourmet meal, saw my family. I tried moving the laptop to another floor so I wouldn't be attached to it, but within an hour or two, it made it's way back downstairs. I didn't leave the house, didn't do any work, have my voicemail set to send callers to a covering doctor. Ah, but here it is, Saturday night, and what am I doing? Yup.... blogging.
So what do you do to unwind? Do you have trouble disconnecting?
Wednesday, December 19, 2012
We Live in a Crazy World
Please, please, I must beg your forgiveness before posting this. Sometimes, I just wish the world made sense, and it doesn't. I should get over it.
There is the story of a psychiatrist in France who was criminally charged with murder because a patient left and then, 20 days later, killed someone. The psychiatrist was found guilty and I believe she paid damages. I think ClinkShrink may write about this on Clinical Psychiatry News in the coming weeks, but for now, I just couldn't resist the sarcastic pull that overtook me when I saw this...the psychiatrist guilty for another person's murder, the horror of our gun laws, and the ridiculous new CPT codes we will all soon be using. If you are touchy about satire, please don't read anymore.
----------------------
French psychiatrist jailed for patient who committed murder
There is the story of a psychiatrist in France who was criminally charged with murder because a patient left and then, 20 days later, killed someone. The psychiatrist was found guilty and I believe she paid damages. I think ClinkShrink may write about this on Clinical Psychiatry News in the coming weeks, but for now, I just couldn't resist the sarcastic pull that overtook me when I saw this...the psychiatrist guilty for another person's murder, the horror of our gun laws, and the ridiculous new CPT codes we will all soon be using. If you are touchy about satire, please don't read anymore.
----------------------
French psychiatrist jailed for patient who committed murder
Here's the missing back story. During the consultation from which the patient
fled, the psychiatrist was trying to figure out whether the several
sentences the patient said about his episode of syphillis constituted
psychotherapy or whether they were related to the medical aspect of the
patient's care. Should she utter supportive words, and tell the patient
he may not have infected all 50 women
he'd slept with [psychotherapy, supportive in nature], or should she
suggest further testing to rule out possible neurosyphillis [medical
intervention]. Would it take long enough to discuss and therefore be 25.1
minutes, so over half of the session would be devoted to counseling, and if
she arranged for transportation to bring the patient back for an LP next
week, well there's the coordination of care, and the documentation
could be punted. Oh, but unfortunately the patient began to talk about his father -- how
mean, uncaring, and critical he'd been which had lead him to seek
solace in the warm sweet bodies of prostitutes and could this relate to
his relationship with his emotionally distant mother? So now the
possibility of time-based medical management was lost, and an add-on code
for psychotherapy became imperative. The patient rambled on. The doctor
suggested they look at other similar relationships, were his sisters
cold? His aunts? What about that
favorite neighbor, Ester? Oh, gosh, the doctor had now gone to 51
minutes of psychotherapy, so close to that 53 minute threshold for a
higher add-on code and so much more reimbursement, when the patient
announced, "I've had awful diarrhea from the medication you've been
giving me?" The doctor could take it no more and tried to sway the
patient to just 2 more minutes of "You must tell me more about your mother!" Angered at his indifference to her lack of concern about his bowel habits, the patient reached into her desk drawer and pulled out the psychiatrist's
semi-automatic weapon, a bushmaster high velocity rifle she kept to fend off both deer and madmen. He ran from
the room while the doctor tried to figure out, was this a 45 minute therapy
session, or could she have missed a moment of reflection, a tiny little
abreaction, something, anything, to get that 52 minutes of therapy to be 53 minutes of add-on
psychotherapy. In the meantime, the patient and the weapon had gotten
far from the hospital, and the doctor realized she had only 5
bullet points on the exam and oddly enough, the
review of the pertinent psychiatric system looked identical to the
mental status exam. Ah! She could comment on gait and get one more bullet
point: "Patient walked quickly, but steadily, away from my office,
bursting into a run, with my bushmaster rifle." She had enough bullet
points on ROS, exam, and past medical, family, and social history to bill a 99213!
The patient ran and ran, firing rounds of ammunition, all
intended to hit tree branches and drop acorns from the sky. It went
well, with the trees raining down an unrelenting supply of acorns until
the ammo ran out. Frustrated, the patient grabbed an axe, hoping his
blows might shake more acorns from the tree and keep up the deluge. An
80 year-old-man, seeing the rifle on the ground picked it up to ask
about whether it was obtained at a show or from a store, and if the
syphillitic patient was legal and rightful owner, when the patient became agitated,
screaming "F*ck the CPT codes, it was a 30 minute session and a 99212 and
that bitch is upcoding," and with that he swung as hard as he could for
the tree, hoping a few scant acorns still remained to flurry down and
pelt his head, when the old man jumped in his way and instead of hitting
the tree, the patient decapitated the old gent. If only that doc had kept her
guns locked and knew her CPT codes.Sunday, December 16, 2012
Please Don't Make Assumptions
Like many, I have been drenched in sadness this weekend. In honor of ClinkShrink's wisdom that media coverage of tragedies leads to more such atrocities, I will talk in generalities.
When a public tragedy happens, it gives us reason to relate it to the issues we naturally advocate for. I am no exception, and I've been posting articles on my own Facebook page in support of gun control. I especially like this article by Nicholas Kristof, "Do We Have The Courage to Change This?"
Mass shootings bring up the issues of gun control, adequate treatment of the mentally ill, and the combination of the two, as President Obama has put it, oh so in-eloquently, “Enforce the laws we’ve already got. Make sure we are keeping the guns out of the hands of criminals… Those who are mentally ill." And finally, there are what I'll call the Out-in-Left Field assumptions.
Let me take it systematically:
The Out in Left Field Assumptions:
It seems to me that sometimes people are quick to make assumptions, to fill in the blanks using their own stories. On Friday, someone I follow on Twitter posted that the perpetrator's mother (at that point, thought to be a school teacher), was probably bullied at school and the son was doing her "dirty work." I was floored at the assumptions that were made there, with no evidence whatsoever, and I no longer follow that person's tweets.
The Problem is The Mentally Ill People and the Care They Are or Are Not Getting:
On a blog called The Anarchist Soccer Mom, a woman posted about her own son's problems. Her 13-year-old is violent, unpredictable, and sometimes dangerous. He has been hospitalized and she's had to hide sharp objects and call the police. Treatment with many medications has not helped, and she's been told by a social worker that unless he gets into the legal system -- presumably by her pressing charges-- little more can be done (note that this is a child who is in treatment, not an adult refusing care) and she finds that answer inadequate (it is). I don't know enough to comment on the quality of her son's care and whether or not there is more that could be done if only the resources were available --she does say she has health insurance. But what troubled me is that the Huffington Post reprinted it with a title asserting that she is the shooter's mom, naming the gunman in the most recent tragedy. I understand that she worries terribly that her child could do something awful and that she is frustrated by the inadequacy of a system that has been unable to help her child, but so far, we don't know that the shooter in question was anything like her son. We've heard he was smart, quiet, withdrawn, and may have had a diagnosis on the autism spectrum. So far, we've heard nothing about violence or hospitalizations. And since I'm asking people not to make assumptions, I will tell you that I am making the assumption that the Huffington Post renamed her piece with a provocative title.
As of this writing, we know little about the mental health history, or care, that the most recent gunman requested or received, and we have reason to believe that his family may have had resources to obtain care for him. In other instances, shooters have been in active treatment, or have had a history of a single, or a few, visits to student mental health centers, sometimes in the remote past. In retrospect, on any case with a mass shooting of strangers, it's obvious that the mental health care rendered was insufficient, but whether there is something that can learned to prevent future such events remains unclear. These shooters tend to be male and isolated -- that would be a lot of people to round up in preventative measures. While I certainly believe that our mental health services are inadequate, we aren't hearing that shooters were people trying desperately to access care but were unable to do so. Sometimes they are people that a mental health professional or an educational institution was concerned about. And while some gunmen have sought treatment at some point and then fallen through the cracks, it's not always clear that having laws that would make it easier to commit someone would make a difference, or that we want to become a society where people can be forced into treatment because they fit a profile. Nevertheless, Newser linked to the Huffington Post anarchist soccer mom's Huffington Post title with the statement,"It's time for a meaningful, nation-wide conversation about mental health. That's the only way our nation can ever truly heal."
Yes, we need better mental health care. And I do think that if we had a kinder and gentler system of involuntary treatment that didn't upset and traumatize people, then there might be a lower threshold to getting help for people, but I'm not sure that would prevent all these tragedies. It's one way we can begin the process of healing, but it's not the only way. Do we ever really heal from something like this?
Keep the Guns Away from the Mentally Ill
On Pete Earley's website, he talks about how troubling it is when a mentally ill person commits a heinous crime because it further stigmatizes his son who is not violent, but has suffered from a psychiatric condition. I'll let you read his post, because I'm not sure I'll do it justice.
Unfortunately, Mr. Obama, I'm not sure how one goes about keeping arms away from the mentally ill. I'm not even sure who those mentally ill are, given that a gazillion people take psychotropic medications and door-to-door surveys show that over half of all people suffer from a psychiatric disorder at some point in their lives. It seems that disturbed people sometimes obtain guns legally because they aren't ill enough to be identified by the system (for example, if they haven't been hospitalized or criminally charged), or they are related to someone who has legal guns and they use those. And people who are well can buy guns and then later become mentally ill, if you think it's an issue of "those people," think again.
It sounds good -- obviously suicidal or homicidal people shouldn't have guns -- but I don't know how it translates into something useful in terms of legislation.
Gun Control
Okay, you can fly a plane into a building, knife multiple people in China, blow up a federal building with fertilizer, or jump off a bridge. We are never going to prevent all murders and suicides, but gun possession allows for a level of lethality that isn't seen in such numbers when people have impulsive violent moments, have had a little too much to drink, or leave their guns where children can play with them, or disturbed people can take them. We probably can't round up every young man who is isolated and distressed, but we probably can question everyone who purchases large amounts of ammunition, or make it illegal to own high-velocity weapons.
Dr. Erik Roskes, a forensic psychiatrist, notes about the astounding number of gun deaths,"Those victims far outnumber the victims in Connecticut, Colorado, etc on an annual basis, and many would not be dead were it not for easy access to handguns. Many more people die due to impulsive shootings than due to the planned acts of the perpetrators of the mass tragedies - yet because they happen one at a time, there are no headlines. It is not too soon - it is never too soon - to rethink our antisocial national approach to weaponry."
I don't know if we'll find out what happened last week, whether this tragedy was planned or impulsive, the result of anger or psychosis, illness or evil, or whether this, or other similar tragedies, are preventable in a society that values the right to bear arms and the right to refuse psychiatric treatment in the absence of stated imminent dangerousness. Making assumptions is not helpful.
Finally
~Yes, we need better access to mental health care, whether or not such care helps prevent tragic, senseless acts that effect many people or one person.
~Perhaps we want to re-think our threshold for involuntary treatments, but that certainly will not capture every potential mass murderer. If we do so, we want a system where accessing treatment is fast, easy, non-stigmatizing, humane, and respectful.
~We need to re-evaluate our gun laws, now.
I'll go back to my sadness now.
Thursday, December 13, 2012
My Very First TweetChat!
I will be one of the two experts, tweeting from @HopkinsMedicine.
@SharecareNow is hosting an expert-led Twitter chat to help you stress-less this holiday. Join the community discussion, bring your questions and concerns and connect with experts who can help you clear the noise and stay calm and cool this holiday season.
Join the chat Friday, 12/14, 1-2 PM Eastern Time (US) on Twitter.
Follow hashtag #Calm&Cool.
Oh, and if you'd like to tell me how you deal with your holiday stress, I'd love to have you comment!
@SharecareNow is hosting an expert-led Twitter chat to help you stress-less this holiday. Join the community discussion, bring your questions and concerns and connect with experts who can help you clear the noise and stay calm and cool this holiday season.
Join the chat Friday, 12/14, 1-2 PM Eastern Time (US) on Twitter.
Follow hashtag #Calm&Cool.
Oh, and if you'd like to tell me how you deal with your holiday stress, I'd love to have you comment!
Monday, December 10, 2012
They'll Come Knocking
Behind all the anxiety of new CPT codes-- because change is hard-- there is not just the angst of more paperwork, or the question of whether gathering specific data distracts from the work of caring for the individual patients. We wonder whether the burden of new billing systems and more documenting for the sake of being able to code like "real doctors" will actually translate to higher reimbursements. More than that, though, there is the fear, which lately does not go unspoken: the fear of doing it wrong and being accused of insurance fraud. Our presenter at a CPT training seminar warned that down-coding is just as fraudulent as up-coding, and my feeling is that we should accurately code the work we do within the confines of the very complex Evaluation and Management schedule, such that our services do get higher reimbursement --- it's difficult to follow but it's either about collecting the right number of bullet points in each category or it's about spending more than 50% of time counseling and coordinating care. Funny, now psychiatrists have to talk more than they listen. Yet everyone I've spoken to says they code low because they don't want to draw attention to their work and don't want to be accused of fraud. I suggested that this is wrong when the doctor is paid a salary and so the hospital collects lower fees. I also think it's wrong when the doctor is out-of-network and the patient's reimbursement, from their health insurance company with those very high premiums and very low reimbursement for expensive psychiatric services, depends on the code.
Some docs are just trying to ignore the upcoming changes, especially those in small private practices. Insurance companies don't typically audit charts of solo practioners who are not in their networks. It's likely rare that Medicare does either, unless perhaps something looks fishy? So some say, "they won't bother me." Others say, they're coding low to stay off the radar, and at least 2 docs I know are opting out of Medicare, because Medicare audits are scary with their $10,000 per claim fines. (Am I right about this?)
Emailed to me today, with the actually title, "They'll Come Knocking":
Subscribe to Compliance
Watch to Steel Against Investigations and Unnecessary Penalties
Do
you know the new definition of fraud? Are you up to
snuff on changes to CPT codes? Big changes are on the horizon. Are you
ready for how they will affect your day-to-day and business practices?
To
survive in our new healthcare environment, staying current on mandates
and preparing adequately for investigations and audits is crucial.Of course this company is selling their services and they are doing it through scare techniques, but still.
Friday, December 07, 2012
The Shrink Rappers in New York: A Little bit of Chaos!
(note, I corrected a zillion typos and added a little)
The Shrink Rappers spoke last night at the New York Public
Library, the mid-town branch, right across from the big library with the
lions. Let me tell you about my
day.
Well, I travelled up with Clink, Roy came later. Clink wanted to take the bus, so we
took the bus. I had been consumed
for two days with creating my CPT coding tutorials, which had kept me up well
into the night, and at 1 AM, I had posted the last three parts of the 4 part series. On the bus, I received three emails telling
me there were multiple sound-tracks of me talking over myself (--somehow Clink
& Roy thought that now everyone would know how they feel…), so that weighed
on me with the mission to get to the hotel and get WiFi as soon after eating
lox & bagel (my NYC must) as
possible.
I started to
work on the talk we were giving at the library that night on my laptop on a bouncy bus when
Clink began laughing. Truth be
told, she emits periodic hamster noises when she’s reading from her iPhone, but
this was a true laugh. A friend of a friend
of Clink's had posted on Facebook, “Hey, tomorrow I get my new
boobs!” I thought this was funny
enough to write about on my own Facebook page, but I inadvertently posted it to
the Shrink Rap Book facebook page instead --one more reason you should Friend us.
We stopped for Bagels & Lox (so much better in New York than in Baltimore), Clink tethered me to her WiFi, and with a
slow connection, it seemed I couldn’t quite post the fixed version of CPT
Coding, Part 2, but later, it seemed I had fixed it. Clink would like credit for uploading to YouTube while I got ready for our talk.
Roy arrived and they want to head to the library, but I was
glued to Shrink Rap & YouTube.
We finally left, with plenty of time to spare, and Roy rushed through
the streets of New York at pace I found hard to keep up with. Why did this have to be the one event
in his life he’s early to? We were
early.
In anticipation of the talk, and with a few friends who’d
asked when I’d be in New York next, I had sent out an email to the few random
people I still know in the City and the surrounding ‘burbs. The numbers have dwindled over the
decades. I tried to make a
reservation at The Bryant Park Grill next to the library, but there were
none available (this was 10 days before).
I tried other nearby restaurants.
Holiday season, no reservations anywhere. Patty from high school sent me a list of places nearby and I
found a Tavern next door with availability, but Yelp described it as a loud
pick-up bar with dirty bathrooms.
An Italian restaurant with a long funny name only three blocks away sounded quiet
and good. I tried to make a
reservation at 9 for 8, instead I got a
reservation at 8:30 for 6, having no idea who was coming. What I didn’t notice was that the
website said “LocationS” (plural) and the different locations had different
names and the name I sent everyone was the restaurant across town. I noticed this at 6:20 pm, just as we
were setting up to talk at 6:30. I also
realized I didn’t have a phone number for Nick, who had said he’d join us at
8:30. I haven’t seen Nick in 20
years. I shot off an email, hoping
he’d see it. He did, but not until after he’d gone to the wrong library and was
headed across town to the wrong restaurant.
I spoke first.
It was a great group, maybe 60-80 people, a full room, and they asked
lots of questions. I noticed a
voicemail had come through on my phone.
As Clink started to talk, I ducked out to listen, and a man beckoned me
over. I leaned in to hear his
question, and he asked “Why did Susan Smith kill her children?” Oh, my. The librarian was also vying for my attention, and the
voicemail was from Patty saying she couldn’t make it.
The talks went well, people had lots of questions for Clink—they
always do, she always has cool stuff to present. She made a video of a SWAT team standoff where the defendent
was tweeting and broadcasting his police negotiations. Roy talked about health information technology, state-run electronic medical record systems, the M3 mental health screen, and increased morbidity, mortality, and expense of health care in people with mental illnesses. The library folks told us were great
and they could have listened to us forever, which might work because we can
talk forever. We were told that
the talks – by the end it was all questions, and questions, and more questions—always
end by 8:30 and this was the first one that had gone on until nearly 9. We left feeling pretty good.
The subsequent
voicemails were from Nick, and then there was Steve’s friend who was at the
restaurant across town, the one which had no reservation for us, but they had kindly
secured him a table for 7 where he was waiting alone. Debbie, from college, came in from Long Island, and she actually made it to part of our
talk, after a quest to find parking and a visit to main library where we
weren’t. Believe it or not, we all ended up at the right restaurant –
Steve’s friend was gracious enough to say it was nicer than the place he’d sat
by himself at the table for 7 – the drinks were good, the food was excellent,
the company superb, and it was Osteria something, the East side one, not the
West side one.
Clink and I are staying in New York and she has quite the
day planned for us. We’re going to
the Museum of Modern Art to see The Scream. We’re eating lunch at Cannibal. And we’re going to see The Anarchist, a play by David Mamet
that opened last week and has gotten such scathing reviews that it’s closing
date is about to be announced. I
hope Clink’s friend of a friend likes her new boobs.
Thursday, December 06, 2012
Tutorials: CPT Coding for Outpatient Psychiatrists for 2013
The way mental health clinicians code their services for insurers is changing on January 1st. A minor thing, a really boring & tedious thing, but I decided I'd learn about it to write about it (oh, I have, but instead of writing, I call it Ranting) and make YouTube how-to videos on how to do the new coding.
Only the new coding takes something that was simple and self-explanatory and makes it really complicated -- it requires courses, manuals with more layers of charts and graphs and algorithms then you want to imagine, and it's all done in a way that has nothing to do with how psychiatry is actually practiced (it's about asking questions to get enough bullet points on your template). I'm seriously considering resigning from the APA over this-- they wanted and supported these changes that make something so simple into a pain, and could potentially be yet one more distraction from taking good care of patients. There are now 21 ways to code a psychotherapy session. However, if you want to learn about the new coding, I'm pleased to report that after hours of technologic hell involving PowerPoint, iPhoto, GarageBand, and iMovie, I now have 4 videos on YouTube about CPT codes for psychiatrists. Thanks to Clink for emailing me a brief how-to list, but in the end I did it all by myself!
It's not looking like the insurance companies have changed their coding for next month, and many people don't know how to do the new coding, so if you're a patient waiting reimbursement, you might want to make sure your therapist/shrink knows to code the new codes (which might not work) and you might want to stay on top of the insurance company. And if you're a mental health professional who gets reimbursed by insurance, you may want to make other plans for that mortgage.
I will tell you that Roy is all in favor of the changes and thinks it's going to lead to much better reimbursements for psychiatry now that we'll be billing like the real docs do.
If you watch these, coffee first. They are really boring. And I think they are only of interest to psychiatrists.
Please do write in the comment section if you find other errors, I will correct them.
Tuesday, December 04, 2012
The Last Day of ACPN by Guest Blogger Dr. Kastenberg!
ACNP Day 3
Rethinking Addictions
It was standing room only at today’s session chaired by
David Kupfer, MD on the updates to the DSM. The changes to three sections were discussed at length: Autism Spectrum Disorder, Schizophrenia
Spectrum, and Addictions. But I
want to focus on the addictions category.
As background, researchers developed the DSM to give one
another standard criteria for psychiatric disorders and a common language. So when you perform a research study to
examine 100 people with major depression, other researchers will know just what
you are describing. The plan
is always to update the information, stay current with new findings, and even
include reliable markers for illness in the criteria.
In keeping with these goals, the substance disorders work
group removed two of the criteria for substance dependence: tolerance and withdrawal.* Tolerance describes the need to
take more of a substance over time to achieve the same effect and withdrawal
describes symptoms that occur when a person abruptly stops a sunstance. These are normal physiologic responses.
Dr. O’Brien emphasized what doctors in the trenches have
been discussing with their patients for years. Being tolerant or experiencing withdrawal to a medication
does not make you an addict.
* They made some other interesting changes too, but those
are not described here.
Monday, December 03, 2012
Day 2 of ACNP by Guest Blogger Dr. Judith Kastenberg
Moviedoc wants to know don't the neuropsychopharmacologists tweet their sessions? They do. Today, I tweeted psychiatry Grand Rounds at Johns Hopkins on Neuropsych testing (#jhhgr) and tomorrow I'll be tweeting a CPT seminar from 6-8 pm (#cpt)
Okay, let me move over and let Dr. Kastenberg blog. She even sent pretty pictures.
---------------------------
ACNP Day 2
This morning’s plenary lecturers showed how nerve cells in
the brain are connected to one another and how those disruptions in those connections
can help us understand disease processes.
We know that neurons communicate with one another by
spitting chemicals into the space between them that act at specific
receptors. Those chemicals are
called neurotransmitters. Our current
models of mental illness suggest that disruptions in this pathway - such as the
wrong amount of a neurotransmitters or the wrong shape of a receptor – are the
source of the problems. And
medications that treat mental illnesses typically restore balance to that
system.
But this research looks at where the neurons are in the
brain. Where do they travel? How do they organize within the
brain? How do messages get from
one part of the brain to another part far away? And does the structure of these pathways explain their
functions?
Scientists now can image many of these pathways and the
images look both structured and complex.
This one by Van J. Weeden at MGH by represents a huge wiring
diagram.
This one by Edward Bullmore at The University of Cambridge
looks like a complex airline flight path map.
Note from Dinah: This looks like something Roy would draw on his iPad.
Sunday, December 02, 2012
Guest Blogger Dr. Judith Kastenberg from the ACNP Annual Meeting
You know how ClinkShrink writes to us about the AAPL (the Amercian Academy of Psychiatry and the Law) conference every year? Our friend and colleague, Dr. Judith Kastenberg in Philadelphia has offered to do a similar guest post about what is going on at the American College of Neuropsychopharmacology (ACNP). From Florida, Judy writes:
Today was first day of the 51st annual meeting of
the American College of Neuropsychopharmacology. Researchers and clinicians founded this working group in 1961
to promote understanding about how drugs work in the brain, identify areas of
controversy in research, identify gaps in knowledge, and brainstorm about
necessary areas of further investigation.
Why then? It
was in the 1950s that the first psychoactive medications were discovered
concurrent with basic science research progress about cellular communication
and ideas about how these medications might act.
The meetings still work to connect basic science research –
what happens in a test tube – with clinical medicine – what happens to real
world patients. Today’s theme at
the meetings explored how stress might influence physical and mental illness.
Common sense tells us that stress influences health. Have a big test in school
tomorrow? You might have a
stomachache before the morning bus.
Thomas Neylan at UCSF reviewed VA healthcare records of
young veterans from Iraq and Afghanistan.
We hypothesize that people with PTSD might be more prone to
“inflammation” as inferred by elevated levels of a marker called C-reactive
protein. So are people with PTSD
also more at risk of developing autoimmune disorders? Dr. Neylan’s data shows that these veterans are more
likely to have certain illnesses like lupus, MS, and inflammatory bowel
disease. There may be other things
at play like a history of sleep deprivation, but the numbers are compelling.
Even rats raised by parents who were traumatized, will act
as if they themselves had been traumatized.
But more on rats in another post.
Friday, November 30, 2012
The Shrink Rappers in The Big Apple
We will be speaking next Thursday, December 6th, at the New York Public Library and we'd love to meet you! We're under a program called The Thought Gallery, which sounds good for a psychiatric thing, right?
Details are HERE. The time is 6:30 pm to 8:30 pm.
The Mid-Manhattan Library is located on the southeast corner of 5th Avenue and 40th Street. It is diagonally across the street from the Research Library (the Library with the lions). We will be on the 6th floor.
Thursday, November 29, 2012
Ranting on KevinMD about CPT Code Changes
I need a new obsession. It may be a few weeks, I still don't know how this new coding works, or what I'm going to tell my patients, or how I'm going to change my invoice system to deal with all the new codes. Over on KevinMD, I outlined all of my angst, plus my frustration with how the new coding deals with Medicare. Please do check out my Rant of the Day.
Tuesday, November 27, 2012
Is There any Hope?
Over on Pete Earley's blog, he's posted a letter from desperate parents who can't get help for their son. Pete, as you may know, is a former Washington Post reporter, author of many books, and a mental health advocate. Yesterday, Pete answered the letter with 10 suggestions. He solicited a panel to take turns responding, and today, I'm the one with suggestions. Here's the letter, then do surf over to Pete's blog and check out the responses, more will be coming all week.
Dear Pete,
We have tried to get our son professional help. I think he has bipolar disorder, although he possibly could have schizophrenia. We know he has an alcohol addiction. He has not cooperated with hardly anything, and we’ve been unable to get him to go to our local mental health center, although officials there said he is eligible for treatment.
We feel like our hands our tied. The few times that we’ve gotten him to a psychiatrist, our son denies that he is sick, won’t take his medicine, and is extremely hostile to doctors for the short time he’s being seen by them. We’ve had him in our house for several months with his erratic moods and high level of anger. Yesterday he asked to go to a homeless shelter and he is now on the streets. If we try to visit him, he runs away.
His dad and I are at the point where we feel resigned that there is no hope nor help for our son. The system has worked against us at every turn … and he needs help. People have recommended “he needs to hit rock bottom” and that we need to wait for him to *want* help. We simply don’t know what to do. Do we wait for him to hit rock bottom on the streets where we know he is not safe?
In our view, the mental health network has been ineffective at best, and is rolling the dice with people’s lives. Now we can see how barriers in the mental illness system keep people from receiving basic services. This has been hell for his dad and me, and I’m sure worse for our son.
If you have any advice please let us know.
-A concerned parent.
Can Psychoanalysis be Coded with the New CPT, E/M Codes?
The
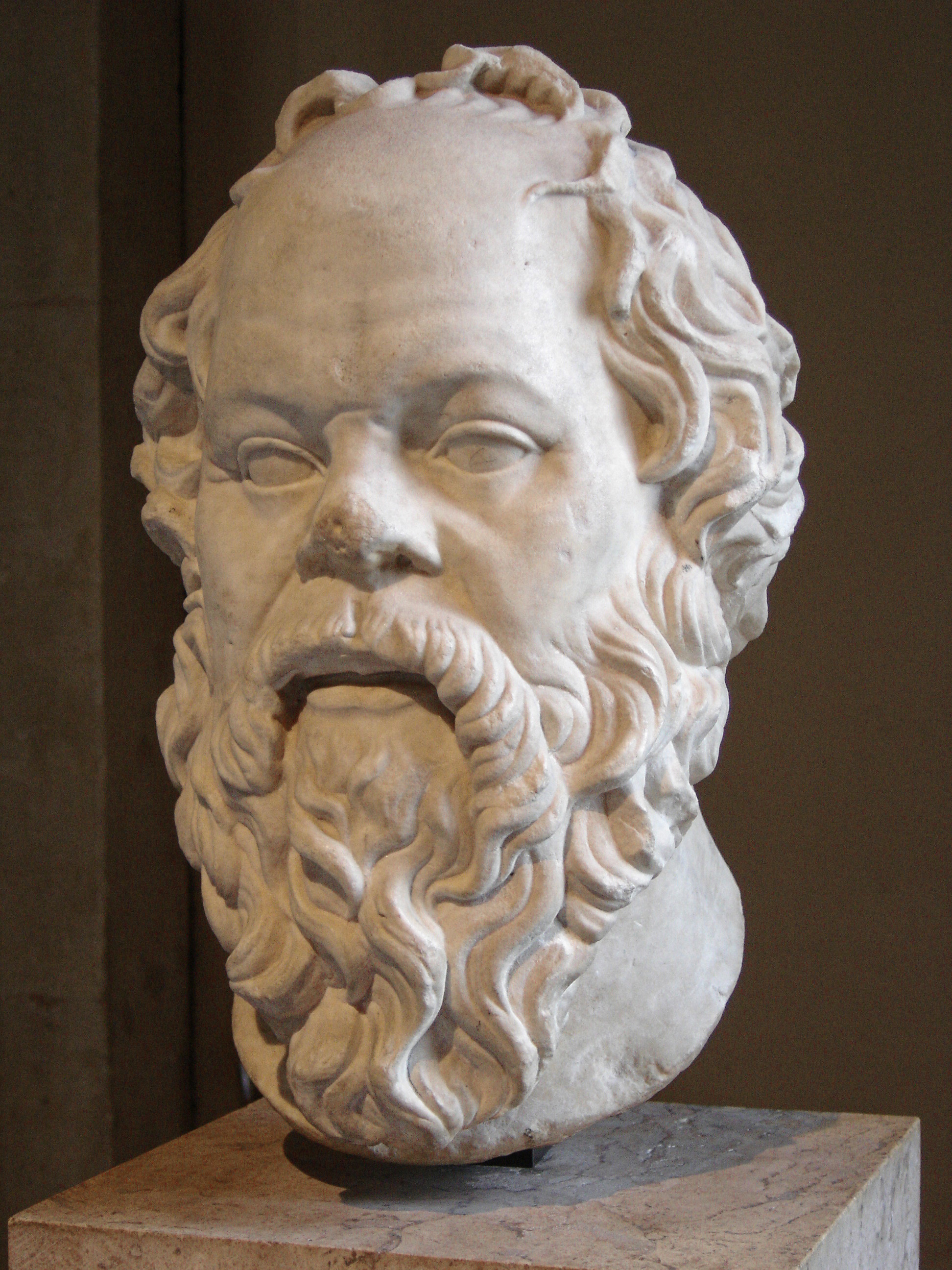
blogger -Psych Practice- who posted on how to figure out an E/M code which I stole
below, did a wonderful job of giving a clear set of directions on how to do this,
though I have to say that I got nauseous half-way through because it is
so long and complex with so many charts, but it does explain it.
S/he wrote a follow-up blog post on how to code for a psychoanalytic
session with Socrates as an example (I was a little confused about the
Speech: Greek, Appearance: Toga, but I then I got it). Anyway, it's
very clever, and it makes the process seem a little less intimidating,
and it does a wonderful job of incorporating the E/M portion of the session into what naturally flows without requiring the therapist to collect irrelevant data for the sake of documentation. I hope it's right. So here's the link to the how to code E/M + add on therapy for the psychoanalysis of Socrates: http://psychpracticemd.blogspot.com/2012/11/em-psychoanalysis-note-monday.html
What this writer doesn't seem to take into account is the proclamation by AMA that the time spent on E/M must be completely distinct from the time spent on psychotherapy. Any one who has ever conducted or had psychotherapy knows, this is not possible. It's like the AMA decided the sky is now purple with orange polka dots. People come in and talk about what's important to them, and if they are depressed and have questions about that Abilify stuff they saw on TV, or are undergoing cancer treatments, or are about to have their knees replaced, that's what they talk about and it's not possible to define one part of a session as "psychotherapy" and instruct them to limit concerns about illnesses & treatments to a specific, time-distinct, portion of the session that is not "psychotherapy." I believe that we have to say that regardless of what Insurers, the AMA, or the APA believe, that it's simply not possible to disentangle the time devoted to the two. The stickiness of the issue is whether insurers/medicare are going to claim that if you have a 53 minute session and document a 99213 E/M code with a 90838 (60 minute psychotherapy add on) that you can't have done that much work seeing patients every hour and are going to insist that the therapy code be for the 45 (38-52 actually) minute shorter, session. For medicare, there is a $45 dollar pay increase if the psychotherapy session goes from 52 minutes to 53 minutes. I'm not the only one who thinks this is all nuts, right?
Monday, November 26, 2012
Practicing My Twittering Tweets
Today, I live tweeted psychiatry Grand Rounds from Johns Hopkins on Traumatic Brain Injury. I've tried to do this before, but I got paged out after just a few tweets. Today, I made it through the whole lecture. I didn't tweet the patient presentation, just the lecture part. I didn't have my laptop, or WiFi access, so I did it from my iPhone on the touch screen where my fat fingers sometimes hit the wrong key. And while the speaker was excellent, she spoke really, really fast, and I missed a bit. I did my best. You can check it out at #jhhgr. My tweets are a bit disorganized and fragmented, but it's not really the venue for precision.
Next week, the Maryland Psychiatric Society will be holding a seminar on how to do the new CPT coding and I'm hoping I can live tweet that. Again, no WiFi, and it will be my fingers flying as fast as they can on my phone. The seminar is much longer than the talk I tweeted today. Maybe the speaker will talk a little slower. So tune in, and if I can, I'll be tweeting the seminar at 6 PM on 12/4 using hashtag #cpt.
Sunday, November 25, 2012
How to Determine and Document an Evaluation/Management Code
With permission, I am stealing this entire post from Psych Practice, a NYC psychiatrist who was kind enough to go through a step-by-step How To Guide for determining and documenting the Evaluation and Management coding for the new CPT codes we'll be using in January. And thank you to Becca who found this for me. Now if someone could translate it into exactly what one needs to do when using these E/M codes in combination with the psychotherapy codes, that would be wonderful.
Let’s look at each of the three components.
1. History:
History is broken into 4 parts, namely, CC, HPI (or Interval History for an established patient), ROS, and PFSH (past medical, family, and social history).
CC is the presenting complaint for that session, and can be related to the diagnosis.
Examples: “Anxiety”, or “F/U for Anxiety”
In case you were wondering, a CC is required for all notes, not just the initial evaluation.
HPI or Interval History is comprised of the following elements:
• Location
• Quality
• Severity
• Duration
• Timing
• Context
• Modifying Factors
• Associated Signs and Symptoms
HPI is considered “ Brief” if it includes 1-3 of these elements, and “Extended” if it includes > 4 elements or 3 stable conditions.
Example: The patient c/o worsening anxiety x 1 week with panic symptoms that occur intermittently, on average once per day, last for 5 minutes, and are brought on unexpectedly by unclear precipitants.
This would qualify as an extended interval history because it includes 4 elements: severity, duration, timing, and context (or 5 if you include modifying factors).
ROS includes pertinent positives and negatives. There are fourteen individual systems recognized by the E/M guidelines:
• Constitutional (e.g., fever, weight loss)
• Eyes
• Ears, Nose, Mouth, Throat
• Cardiovascular
• Respiratory
• Gastrointestinal
• Genitourinary
• Musculoskeletal
• Integumentary (skin and/or breast)
Social History (SH): An age appropriate review of the patient’s past and current activities which may include significant information about:
An example to clarify: In order to be able to bill for an E/M 99213 code, you need to refer to Table 1, above, where you note that the required history is an extended problem focussed history. In order to determine what constitutes an extended problem focussed history, you refer to Table 2, where you note that a brief HPI and 1 ROS are enough to qualify.
2. Psychiatric Medical Exam -Includes the following elements:
• Speech
• Thought Processes
• Abnormal/Psychotic Thoughts
• Associations
• Judgement
• Orientation Time/Place/Person
• Memory
• Attention Span/Concentration
• Language
• Fund of Knowledge
• Mood/Affect
• General Appearance
• Muscle Strength/Tone
• Gait/Station
• Vital Signs (> 3)
• Other
Example:
• Speech-normal rate, rhythm, volume, speaks English with an accent
• Thought Processes-coherent
• Judgement-good
Let’s look at how each of these parts is determined.
Example: “Patient with h/o anxiety, worsening over the last week,” would generate 2 problem points.
Example: “Ordered PFTs for SOB,” would earn 1 data point.
Example: “Worsening anxiety,” would qualify as moderate risk.
First, the History:
The Interval History includes at least 4 elements-severity, duration, timing, and
context. This makes it extended.
The ROS includes 3 systems, GI, respiratory, and psychiatric.
The PFSH includes one element of Social History, namely, that the patient is a graduate student in Physics. Listing the allergies as NKDA may also qualify as one element of PFSH.
Extended HPI, 2 ROS, and 1 PFSH qualify as a detailed history.
Now the Psychiatric Exam:.
6 elements are noted, speech, thought, judgement,
fund of knowledge, affect, and general appearance.
And the MDM:
Anxiety is an existing problem for the patient. Since it is worsening, this earns 2 problem points.
Referring to Table 6, it is clear that there are no data points.
And finally, risk. A chronic illness with mild exacerbation is considered moderate
risk.
Referring to Table 4, levels of MDM:
E;M Coding, in All Its Glory
There are three key components to E&M level of care: history, exam, and medical decision making. Each of these components has requirements for meeting the various levels of care. You need 2 out of 3 of these components to reach a specified level of care. For example, if you have an extended problem focussed history, but only 2 exam elements, you can still meet criteria for a 99213 provided your medical decision making is of low complexity. It sounds confusing, but it’ll become clearer as we move along. The details for each of these components follow, after which I’ll give some examples.
There are three key components to E&M level of care: history, exam, and medical decision making. Each of these components has requirements for meeting the various levels of care. You need 2 out of 3 of these components to reach a specified level of care. For example, if you have an extended problem focussed history, but only 2 exam elements, you can still meet criteria for a 99213 provided your medical decision making is of low complexity. It sounds confusing, but it’ll become clearer as we move along. The details for each of these components follow, after which I’ll give some examples.
Table 1
Level Of Care Requirements (2 out of 3 needed)
Level of Care
|
Hx
|
Exam
|
MDM
|
99212
|
Problem Focussed
|
1-5
|
Straightforward
|
99213
|
Extended Problem
Focussed
|
>6
|
Low Complexity
|
99214
|
Detailed
|
12 from 2 or more
organ systems
|
Moderate
Complexity
|
99215
|
Comprehensive
|
2 from each of 9
organ systems
|
High Complexity
|
Let’s look at each of the three components.
1. History:
History is broken into 4 parts, namely, CC, HPI (or Interval History for an established patient), ROS, and PFSH (past medical, family, and social history).
CC is the presenting complaint for that session, and can be related to the diagnosis.
Examples: “Anxiety”, or “F/U for Anxiety”
In case you were wondering, a CC is required for all notes, not just the initial evaluation.
HPI or Interval History is comprised of the following elements:
• Location
• Quality
• Severity
• Duration
• Timing
• Context
• Modifying Factors
• Associated Signs and Symptoms
HPI is considered “ Brief” if it includes 1-3 of these elements, and “Extended” if it includes > 4 elements or 3 stable conditions.
Example: The patient c/o worsening anxiety x 1 week with panic symptoms that occur intermittently, on average once per day, last for 5 minutes, and are brought on unexpectedly by unclear precipitants.
This would qualify as an extended interval history because it includes 4 elements: severity, duration, timing, and context (or 5 if you include modifying factors).
ROS includes pertinent positives and negatives. There are fourteen individual systems recognized by the E/M guidelines:
• Constitutional (e.g., fever, weight loss)
• Eyes
• Ears, Nose, Mouth, Throat
• Cardiovascular
• Respiratory
• Gastrointestinal
• Genitourinary
• Musculoskeletal
• Integumentary (skin and/or breast)
• Neurological
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/Immunologic
Even in Psychiatry, it is possible to review more than one organ system.
Example: ROS positive for GI upset, SOB, diaphoresis, and dissociative feelings.
This example could arguably include GI, Respiratory, and Psychiatric. However, it’s unclear what the liability is if you’re calling SOB respiratory, and then not listening to the patient’s lungs.
PFSH -Pertinent Past Medical, Family, Social History
Past Medical History: a review of past illnesses, operations or injuries, which may
include:
Family History (FH): a review of medical events in the patient’s family which may include information about:
• Psychiatric
• Endocrine
• Hematologic/Lymphatic
• Allergic/Immunologic
Even in Psychiatry, it is possible to review more than one organ system.
Example: ROS positive for GI upset, SOB, diaphoresis, and dissociative feelings.
This example could arguably include GI, Respiratory, and Psychiatric. However, it’s unclear what the liability is if you’re calling SOB respiratory, and then not listening to the patient’s lungs.
PFSH -Pertinent Past Medical, Family, Social History
Past Medical History: a review of past illnesses, operations or injuries, which may
include:
- Prior illnesses or injuries
- Prior operations
- Prior hospitalizations
- Current medications
- Allergies
- Age appropriate immunization status
- Age appropriate feeding/dietary status
Family History (FH): a review of medical events in the patient’s family which may include information about:
- The health status or cause of death of parents, siblings and children
- Specific diseases related to problems identified in the Chief Compliant, HPI, or ROS
- Diseases of family members which may be hereditary or place the patient at risk
Social History (SH): An age appropriate review of the patient’s past and current activities which may include significant information about:
- Marital status and/or living arrangements
- Current employment
- Occupational history
- Use of drugs, alcohol or tobacco
- Level of education
- Sexual history
- Other relevant social factors
Example: Patient is a graduate student in Physics, about to defend his dissertation.
Note: You DO NOT need to re-record a PFSH if there is an earlier version available on the chart. It is acceptable to review the old PFSH and note any changes. In order to use this shortcut, you must note the date and location of the previous PFSH and comment on any changes in the information since the original PFSH was recorded. For example, if you are seeing an established patient in the office you can write: “Comprehensive PFSH which was performed during a previous encounter was re-examined and reviewed with the patient. There is nothing new to add today. For details, please refer to my previous note in this chart, dated 11/23/2004.” ( From EMUniversity.com)
Note: You DO NOT need to re-record a PFSH if there is an earlier version available on the chart. It is acceptable to review the old PFSH and note any changes. In order to use this shortcut, you must note the date and location of the previous PFSH and comment on any changes in the information since the original PFSH was recorded. For example, if you are seeing an established patient in the office you can write: “Comprehensive PFSH which was performed during a previous encounter was re-examined and reviewed with the patient. There is nothing new to add today. For details, please refer to my previous note in this chart, dated 11/23/2004.” ( From EMUniversity.com)
Table 2
Levels Of History (3 out of 3 needed)
Level of Hx
|
HPI
|
ROS
|
PFSH
|
Problem
Focussed
|
Brief
|
None
|
None
|
Extended Problem
Focussed
|
Brief
|
1 System
|
None
|
Detailed
|
Extended
|
2 Systems
|
1
|
An example to clarify: In order to be able to bill for an E/M 99213 code, you need to refer to Table 1, above, where you note that the required history is an extended problem focussed history. In order to determine what constitutes an extended problem focussed history, you refer to Table 2, where you note that a brief HPI and 1 ROS are enough to qualify.
2. Psychiatric Medical Exam -Includes the following elements:
• Speech
• Thought Processes
• Abnormal/Psychotic Thoughts
• Associations
• Judgement
• Orientation Time/Place/Person
• Memory
• Attention Span/Concentration
• Language
• Fund of Knowledge
• Mood/Affect
• General Appearance
• Muscle Strength/Tone
• Gait/Station
• Vital Signs (> 3)
• Other
Table 3
Levels of Psychiatric Exam
Level of Care
|
# elements on exam
|
99212
|
1-5
|
99213
|
>6
|
99214
|
12 from 2 or more organ
systems
|
Example:
• Speech-normal rate, rhythm, volume, speaks English with an accent
• Thought Processes-coherent
• Judgement-good
• Fund of Knowledge-excellent
• Affect-anxious
• General Appearance-messy hair, not wearing socks, otherwise well-groomed.
This example includes 6 Psychiatric exam elements, and would therefore qualify as a 99213 level of care exam.
3. Medical Decision Making - EMUniversity MDM
This part is a little tricky. You can check out the link, but I’ll try to summarize.
It seems as though you can raise the E/M code depending on the complexity of your decision-making. But how the complexity is determined is, well, complex.
Referring back to Table 1, you’ll note that there are 4 levels of MDM:
Each of these, in turn, is broken down into 3 parts:
• Affect-anxious
• General Appearance-messy hair, not wearing socks, otherwise well-groomed.
This example includes 6 Psychiatric exam elements, and would therefore qualify as a 99213 level of care exam.
3. Medical Decision Making - EMUniversity MDM
This part is a little tricky. You can check out the link, but I’ll try to summarize.
It seems as though you can raise the E/M code depending on the complexity of your decision-making. But how the complexity is determined is, well, complex.
Referring back to Table 1, you’ll note that there are 4 levels of MDM:
- Straightforward
- Low Complexity
- Moderate Complexity
- High Complexity
Each of these, in turn, is broken down into 3 parts:
- Problem Points
- Data Points
- Risk
So get ready for more tables.
Table 4, Levels of MDM
(2 out of 3 needed)
Overall MDM
|
Problem Points
|
Data Points
|
Risk
|
Straightforward
|
1
|
1
|
Minimal
|
Low Complexity
|
2
|
2
|
Low
|
Moderate Complexity
|
3
|
3
|
Moderate
|
High Complexity
|
4
|
4
|
High
|
Let’s look at how each of these parts is determined.
Table 5
Problem Points
Problem
|
Points
|
Self Limited or Minor (max of 2), e.g. common cold
|
1
|
Established Problem, Stable or Improving
|
1
|
Established Problem, Worsening
|
2
|
New Problem, no additional w/u planned, (max of 1)
|
3
|
New Problem, additional w/u planned
|
4
|
Example: “Patient with h/o anxiety, worsening over the last week,” would generate 2 problem points.
Table 6, Data Points
Data Reviewed
|
Points
|
Review or order clinical labs (1 pt total, not 1 for each)
|
1
|
Review or order radiology (except echo or heart cath)
|
1
|
Review or order medicine tests (e.g. PFTs, EKG)
|
1
|
Discuss test with performing physician
|
1
|
Independent review of image, tracing or specimen
|
2
|
Decision to obtain old records
|
1
|
Review and summation of old records
|
2
|
Example: “Ordered PFTs for SOB,” would earn 1 data point.
Table 7, Risk-only need 1 from any level, use highest risk present (from EMUniversity.com)
| Minimal Risk | Low Risk | Moderate Risk |
High Risk
|
•One self-
limited or minor
problem (e.g.,
cold, insect
bite, tinea cor-
poris)
•Labs: EKG, E EG, CXR, UA, Ultrasound Echo, KOH prep •Rest •Gargles •Elastic bandages Superficial dress- •ings |
•Two or more self-
limited or minor
problems
•One stable chronic ill- ness, (e.g., well con- trolled HTN, DM2) •Acute uncomplicated illness or injury (e.g., cystitis/ rhinitis) •Physiologic tests without stress •Non- cardiovascular imaging with contrast •Over the counter drugs •Minor surgery without •risk factors •PT/OT •IV fluids without additives |
•One or more chronic
illness, with mild
exacerbation or
progression
•Two or more stable chronic illnesses •Undiagnosed new problem with uncer- tain prognosis (e.g., lump in breast) •Acute illness with systemic symptoms (e.g., pyelonephritis, colitis) •Physiologic tests with stress •Prescription drug management •Minor surgery with risk factors •Elective major surgery without risk •factors •IV fluids with additives |
•Chronic illness with
severe exacerbation
or progression
•Illness with threat to
life or bodily function
(MI, ARF, PE)
•Abrupt change in
neurological status
(TIA, weakness)
•Cardiovascular
imaging with contrast
(arteriogram, cardiac
cath) with risk factors
•Elective major
surgery with risk
factors
•Emergency surgery •Parenteral controlled substances •Drugs requiring intensive monitoring for toxicity •Decision for DNR or to de-escalate care |
Example: “Worsening anxiety,” would qualify as moderate risk.
Now let’s look at a complete note, and determine which E/M level it qualifies for:
Einstein, Albert DOB: 03.14.1879 Date of Visit: 11 11 12
Start:1:45p Stop:2:30p Total face to face time: 45 min
CPT: 90836, E/M ?????
CC: F/U for Anxiety
Interval Hx: The
patient c/o worsening anxiety x 1 week with panic symptoms that occur
intermittently, on average once per day, last for 5 minutes, and are
brought on unexpectedly by unclear precipitants, in the context of his
upcoming dissertation defense.
ROS: Pt. reports intermittent panic symptoms, including GI upset, SOB, and dissociative feelings.
PFSH: Patient is a graduate student in Physics.
PME:
- Speech-normal rate, rhythm, volume, speaks English with an accent
- Thought Processes-coherent
- Judgement-good
- Fund of Knowledge-excellent
- Affect-anxious
- General Appearance-messy hair, not wearing socks, otherwise well-groomed.
Dx: Anxiety NOS 300.00
Current Meds: Zoloft 100mg qd.
Side effects: No side effects or adverse reactions noted or reported.
Allergies: NKDA
Labs: ordered-none, reviewed-none
Psychotherapy Note: Discussed
with patient his automatic thoughts, and the specific concerns he has
about his dissertation defense. Reviewed relaxation techniques with
patient.
Plan:
- Continue current medication
- f/u 1/week psychotherapy
First, the History:
The Interval History includes at least 4 elements-severity, duration, timing, and
context. This makes it extended.
The ROS includes 3 systems, GI, respiratory, and psychiatric.
The PFSH includes one element of Social History, namely, that the patient is a graduate student in Physics. Listing the allergies as NKDA may also qualify as one element of PFSH.
Referring back to Table 2, History:
Level of Hx
|
HPI
|
ROS
|
PFSH
|
Problem
Focussed
|
Brief
|
None
|
None
|
Extended Problem
Focussed
|
Brief
|
1 System
|
None
|
Detailed
|
Extended
|
2 Systems
|
1
|
Extended HPI, 2 ROS, and 1 PFSH qualify as a detailed history.
Now the Psychiatric Exam:.
6 elements are noted, speech, thought, judgement,
fund of knowledge, affect, and general appearance.
And the MDM:
Anxiety is an existing problem for the patient. Since it is worsening, this earns 2 problem points.
Referring to Table 6, it is clear that there are no data points.
And finally, risk. A chronic illness with mild exacerbation is considered moderate
risk.
Referring to Table 4, levels of MDM:
Overall MDM
|
Problem Points
|
Data Points
|
Risk
|
Straightforward
|
1
|
1
|
Minimal
|
Low Complexity
|
2
|
2
|
Low
|
Moderate Complexity
|
3
|
3
|
Moderate
|
High Complexity
|
4
|
4
|
High
|
In this case, the overall MDM would be of Low Complexity, since 2 out of 3 elements are needed.
To sum it all up, we look at Table 1, Levels of Care:
Level of Care
|
Hx
|
Exam
|
MDM
|
99212
|
Problem Focussed
|
1-5
|
Straightforward
|
99213
|
Extended Problem
Focussed
|
>6
|
Low Complexity
|
99214
|
Detailed
|
12 from 2 or more
organ systems
|
Moderate
Complexity
|
99215
|
Comprehensive
|
2 from each of 9
organ systems
|
High Complexity
|
Since there is a detailed history, but only 6 exam elements and MDM of low
complexity, this visit would qualify for a 99213 E/M code.
Now, if the patient also carried a diagnosis of depression, and this was stable, this
would earn a total of 3 problem points, 2 for the worsening anxiety, and 1 for the
stable depression. And 3 problem points would move the MDM up to moderate
complexity. And since only 2 out of the 3 key components are required for level of
care, a detailed history and MDM of moderate complexity would qualify as a
99214, which is reimbursed at a higher rate.
Overall, this is a pretty complicated business. It adds extra work to note-writing,
and it’s not really suited to Psychiatry, and certainly not to high frequency
psychotherapy or psychoanalysis. And I suspect that since this is completely new,
and doesn’t fit neatly into nice little well-established, categorized boxes, insurance
companies will also be confused about it. Or the’ll say they are so they can
withhold payment.
Labels:
billing,
coding,
cpt,
E/M,
practice,
psychiatry,
psychotherapy
Subscribe to:
Posts (Atom)