Or:
I Can't Think for Myself
Or:
One Great Way to Kill Trees
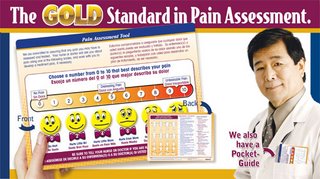
At the institution where I work, there is a requirement by JCAHO that all patients be assessed for pain. What this means, in practical terms, is that every patient at every visit in every department of the hospital is given a form and asked to mark off on a numerical scale how severe their pain is. For patients who can't negotiate that, there are smiley-to-frowny faces drawn and one can circle the face that best approximates one's degree of pain. Unlike the photo depicted above, my institution does not have the scale in color, and our smiley faces do not wear bow ties. You must sign the form at the bottom. I don't know what happens if you refuse, and the form is placed in your chart. We won't discuss what this does to the size of the charts, but hey, they pay me to be here.
I'm a psychiatrist, everyone who walks in the door, at least for the first time, is in pain. No No No No! Not that kind of pain, it has to be physical pain or it doesn't count! Does your body hurt? Now if the pain is more than a 3 out of 10, the patient is to be asked if they want to see a doctor. Oh, I am a doctor. 8 out of 9, maybe 9, It's that arthritis or maybe the chronic migraine. Yup, they have medicine for it. Okay, so now it's checked, they've seen the doctor, the sheet is signed, and it gets filed in the chart. Three cheers for us, we're JHACO compliant. Damn the trees, that's what Oregon's for.
So a patient comes to see me. The patient, John YoungGuy, is 27 years old. He has no significant medical or surgical history, he's here at the psychiatric clinic to get his mental illness treated. He's not in any physical pain (--He signed so it's a fact). The next week, Mr. YoungGuy returns to see me. I should ask him if he hurts? Why would he hurt? Wasn't I listening last week when he said he was healthy and had no pain. Really, he circled the zero and signed. Do I think he wouldn't tell me if he'd broken an arm on Saturday? By the fifth visit, by the fifth request to look at the demeaning smiley faces and sign off of that really, truly, he's not in any physical pain, might Mr. YoungGuy wonder if I'm not listening? If I'm not anything other than some idiot RobotShrink who sits there with a checklist (yup, I do, but at least a few of those questions are relevant, but trust me, the state-mandated 90 med check doesn't count if it isn't written up on the yellow sheet of paper).
I believe the intent of the mandate was good. Attention to pain, treatment of pain-- they are important things in medicine. The kneejerk phenomenon of signing off on a condescending smiley-face form, however, creates a culture where the goal is Compliance with regulatory agencies, not one of caring, attentiveness, creative solutions, or even of compassion. We shouldn't neglect pain, we (meaning all of us form-filler-outers from the orthopedist to the psychiatrist to the dermatologist) should enable relationships of trust and openness where the patient tells us they are in pain, and we address it as best we know how.
By the way: I lied. I never fill the forms out, they go straight into the trash, unchecked, unsigned. I feel way too foolish to even ask. Please don't tell anyone. You can, I hope, feel my pain.
--And by the way, has anyone seen Roy?
23 comments:
Great post. I want to write a better comment on this, but for now - just a couple of things. It sounds like your institution is trying to mimick the NHS in tree-killing by way of useless forms. We don't do that at all! And none of my doctor's offices do that, either. I very much agree that pain is the 5th vital sign and should be assessed with vitals...but not have the patient circle the number and sign a form, each and every time you see them. I do think that pain gets overlooked in some situations, which is why I'm glad they have pushed it to be the "5th vital sign."
But even more importantly, is the part where they say, "Pain is whatever the patient says it is." This is the most important statement on the entire topic. How many times do ER nurses and docs roll their eyes at patients because they don't believe their pain? (I'm not saying they all do this, by any means - but I know how many times a day the discussion of 'drug seeking pain patient' comes up in the ER setting! I worked there, too!) When I went to the ER for the very first time - 8 days into my headache - the PA asked me what my pain was on a scale of 1-10 where 1 was little or no pain, and 10 was the "worst pain imaginable - like a train ran over your legs and cut them off." She had no right to say that. First of all, say a train does run over my legs and cut them off - I might not even feel it if they sever the right nerves...or I might die - and not feel it. And I know I'm being absurd here. But the fact of the matter is that a "10" is not the "worst pain imaginable" - but rather it is MY worst pain. So my 10 won't be the same as your 10 or anybody else's 10. But nobody can say to me, "Oh you don't have a level 10 migraine....you're not crying and you can sit up and have a mild conversation." That's right - I might not be crying and I might be sitting up having a quiet conversation, but my head is still a 10 to me if that's what I say it is. And I don't throw 10's around as a joke - and a 10 for a headache is different than a 10 I'd rate for joint pain and other things.
But anyway, I ramble and/or digress - what I want to say is that the most important part out of the whole mandate is that "pain is whatever the patient says it is." Yes, patients do lie. But drug addicts can feel pain and get sick, too. And sometimes we might seriously doubt that someone feels the pain they say they feel. (Hell, I doubt it quite a lot sometimes....) BUT - we still have to believe them - the pain is what they say it is. How it is treated is a whole different story. But validating pain is important.
Sorry if that's scattered and not written well. I'm exhausted, but really wanted to write that. I have gobs of stuff written on this topic on the internet....it's one of my favorites.
But I still agree that you shouldn't have to have patients fill out that dumb form every time you see them. I like the theory - but not the way you are being forced to carry it out!
Take care,
Carrie :)
just imagine trying to get women in active labor to pick a pain level on a scale of 1-10. They will scream at you if you try.
I agree that we shouldn't ignore pain. But pain isn't the "5th vital sign". Signs are, by definition, things that are objective. Pain is, by its very nature completely subjective. Also, vital signs are things that if they're bad, can kill you. I have a headache (probably about 5/10... bad, but not excruciating), but I'm not going to die from it.
Pain is a symptom of something going on. We need to pay attention to it and to treat it, but it isn't always the most important thing, and I feel like the current emphasis on pain portrays it as the most important thing.
Besides, I think that there are really only 3-4 grades of pain. Minimal/absent, mild, moderate, and severe. Anything else is just busy work.
Scalpel is an ER doc - they are trained to assess people's pain FOR them. He also thinks that headaches are a psychiatric problem and are not real - and that they certainly do not deserve to be treated in an acute inpatient setting - no matter how bad. I'd like to see him live with the pain in my head or the cluster headaches I get sometimes 6 or more times a day. Women who have had children in natural childbirth say that their clusters hurt them worse than delivering that baby. And I haven't had kids yet - but I can say that clusters are the worst thing I have ever experienced in terms of pain. We have our own pain scale that we developed in the cluster headache world, called the Kip scale (because the guy who made it up is named Bob Kipple) - I'll post it later because I have to leave in a minute here. But I can't even sit down if I have a cluster. If I am sitting, I am usually rocking or shaking. I have kicked walls and nearly broken my foot because of the pain of a bad cluster attack....it is excruciating. I know people who have had half their teeth ripped out because they thought that was the cause because that branch of the trigeminal nerve is so extremely painful for them.
But Scalpel would assess a cluster patient as insignificant.....and albeit, I'm basing this on a discussion I had with him on headaches over at Dr. A's blog quite awhile ago - and it was a very ugly discussion.
Pain is what the patient says it is. Unless somebody else has been in my body, they can't tell me how my pain is on a 1-10 scale. And I can't tell anybody else what their's is, either... With the exception of my babies, since they can't tell me - and we have a scale to rate their pain, which we must do at least once a shift - or any time we give a pain med or do any other intervention....
Take care,
Carrie :)
At the risk of sounding like a spammer I have a suggestion for alternatives to remedy some pains that you may not be aware of. My problem was a herniated disk in my neck. I invented and patented the SquidFace and ComfyRest pillows to relieve my neck pain. These pillows enable me to lie facedown comfortably and breathe without turning my head to the side. Unexpected benefits of these pillows are snoring relief; neck, shoulder and back muscle tension relief; scoliosis, sinus, migraine, ear pain, snoring and more while using faceup and sideways. Stomach sleepers are finding their backs feel better after using these pillows. Hopefully this can help others. Many of the benefits are on my website. www.SquidFace.com
EEK, I loved this post. Especially your singular wit. "Do you want to see a doctor?...." As a paramedic pain assessment was something we often tried to do because sometimes that is the only reason someone would call us. And as the other commentator stated it is SO subjective it is ridiculous. The man who had bilateral open ankle fractures comes to mind. He was calmer tham the firefighters. ("can't you give him some morphine or something"?) Sorry officer this isn't Nam. To the man with the splinter in his finger, "Can't you give me some morphine or something?"
I would think that pain assesment in the mentally ill would be very challenging, depending on the case. And besides as you said darling you think from one visit to the next they would tell you anyway. EEK EEK. abf PS and no I haven't seen Roy
abf Thanks for the iguana. And the relativism of pain reminds me of the problem I have with numerical mood scales. If someone rated their mood as a '4' you might think they're basically OK, but that number is meaningless without context. If you knew that over the past three years that patient had only had one '4' day and that the average mood was 6 or 7 with almost no variation, you would know there was something unusual going on. An individual number without context tells you nothing because of the subjective nature of the symptom.
Mood scales, used in properly trained patients, can be very helpful. However, I'm not a researcher, I'm satisfied with the overall "I'm very depressed" (for a description of mood) at the beginning of treatment and "Fine" at the end.
Sometimes I ask patient's "How's your mood" to get an answer of "7." 7? I could explain the scales used, make sure the patient and I are on the same page, that his 7 is my 7, but usually I'm left to say "so, like what does that mean?". Happy, sad, wonderful, miserable, those are all just great.
I'm with MWAK for pain: None, mild, moderate, severe.
The whole point of the scales is to quantify it to bring some validity to what you've all pointed out is a very subjective, difficult-to-be quantified experience.
Perhaps it's not so useful. As Carrie has pointed out, it really isn't helpful to say to someone "You don't hurt" or "You don't hurt THAT much."
"It hurts a whole lot, doc" may be more useful than "10."
I just wish I wasn't being asked to fill out irrelevant paperwork.
And, ABF, I love you too.
If you have to assess pain, why not just ask the person to describe the pain? I'd rather hear someone say "It feels like someone is driving an ice pick through my eardrum" than "8 out of 10."
The only reason I can see for asking people to rate their pain on a scale of 1-10 is that it makes research easier. But on the other hand, it's well known that people avoid the anchors on this type of scale, so you'd just end up with a bunch of data clustered in the middle.
On mood ratings--my favorite is when someone says "I'm feeling good: 4 out of 10." I guess 10 must be full-blown mania?
For the record, in shrink terms:
mood scales
5 is 'normal' neither depressed nor elated, even-keeled, Fine. It's where shrinks think people should be, the goal of treatment.
1 is horribly horribly depressed
10 is incredibly euphoric
so, if you're a little sad, probably a 4.
6 is happy, a little elated, where I like to live.
7 is clearly elated.
If you're feeling Wonderful, it's not a 5.
Words--- I love words-- work better for clinical purposes.
Actually I think we need a Shiny Happy Pain Scale.
My word verification: bfraud
I kid you not.
"But I can't even sit down if I have a cluster. If I am sitting, I am usually rocking or shaking. I have kicked walls and nearly broken my foot because of the pain of a bad cluster attack....it is excruciating...but Scalpel would assess a cluster patient as insignificant"
Actually, if you had read it, my scale would assess you at an 8/10. That's exactly where I was right before my root canal, btw. 8/10 is pretty miserable, but it can be worse.
I totally agree with midwife with a knife; the concept of pain as a fifth vital sign is ridiculous. A guy with a toothache or a woman with a chronic recurrent headache may report "10/10" pain, but as long as there is at least one patient with a marked abnormality of any of the actual vital signs in the department, the pain patients can wait without risk. So pain isn't really that vital, is it?
EEK, I thought she was a chameleon. Are you sharing her? She is a comfort.
Midwife should be informed that when paramedics ask people to rate pain they usually quantify ten should be the worst pain you ever felt,for women like labor.
As for rating mood that I would have a hard time with. I did see a woman with neck pain once. No trauma but she said that it was an alien that now lived in her neck causing the pain. Oh and the woman who told me that she called the plumber, but she really needed a gynecologist.
Enjoy Liz (my son's name for her) and I stll love you. abf
I am here. Was too busy the last 4-5 days so didn't even check my email until last PM.
Great post. I like Gerbil's idea of just describing the pain. Problem with not having a number is that it is hard to write an order that says Percocet 5/325 ii po q4h prn for pain="like an icepick through my eye". How about a 1-10 scale, but instead of smiley/frowny faces, use little icon images, like:
2-being hit with pillow in the face
4-stubbed toe
7-missed the nail while hammering and hit thumb
8-ice pick in the eye
10-leg bent at impossibly acute angle, with jagged shard sticking out
And re Midwife and Scalpel's (sounds like a bizarre vaudeville act) comments about pain not truly being "vital"... au contraire. You can die from a pain of 10, as severe, inescapable pain can be lethal because people would sometimes rather kill themselves than endure it. Because such a death would be preventable, that makes a pain rating "vital" (IMO).
"You can die from a pain of 10, as severe, inescapable pain can be lethal because people would sometimes rather kill themselves than endure it."
That is a manipulative technique we often hear. That'll buy them a Psych consult, but it isn't going to give them carte blanche to automatically receive magadoses of narcotics every time they show up to the ER forever.
I loved your pain scale though. Very funny (but true)!
Carrie, your comment about pain as the "5th vital sign" is quite interesting. When I was working as a medic overseas this summer, pain was often used as a gauge to figure out where a patient was at. Vitals might all be normal, but at the end of the day, when we couldn't even lay a finger on the patient without him/her writhing (is that the right word?) in pain, I knew there was clearly something wrong.
That being said though, there were several patients that I saw several times over the 6 weeks that I worked who were drug-seeking, and really had a good "act" ready for the medics when we were called. Maybe one of the three shrinks, or someone else, can comment on how a practitioner is able to discern whether the patient is looking for narcotics, or is just in a LOT of pain... No one ever clarified that issue for me, I guess the reason being that the medics I worked with saw these people regularly, and knew their schtick.
BTW, my computer still doesn't work, so I'm 3 podcasts behind. Hopefully I'll get up to date before the summer!
Roy: I think you misunderstood. I wasn't saying that pain isn't important or that treating it isn't important, in fact I said it should be treated. I was just saying that it isn't really a vital sign in the same sense that temperature, heart rate, respiratory rate, blood pressure, and O2 saturation (the real 5th vital sign) are.
midwife- true, not an actual "vital" sign, any more than depression, or nausea, or dizziness. It would be nice to be able to apply some type device, like Bones' tricorder, and be able to objectify the amount of pain signal traveling up the spine.
How can you tell "true" pain? The most reliable way is to just ask. Any other way is too unreliable and risks not treating "true" pain. I think folks get too caught up in trying to "catch" people who are faking pain.
Sure, it happens, but how many people with untreated pain (thinking they are faking) is acceptable in order to prevent, say, a hundred fakers from getting their fix?
How a practitioner is able to discern whether the patient is looking for narcotics:
1) "I lost my prescription"
2) "My prescription was stolen"
3) "I'm on vacation, and even though my Dilaudid is the only thing that keeps me from killing myself every day, I happened to leave my medication at home. I must have forgotten it."
4) "My last vicodin prescription was two months ago" (but not according to the pharmacist at Walgreens or your physician, who state that you were given and filled a prescription 2 days ago.
5) "I haven't been to the ER for my back pain in 2 months" (This ER, you mean. The one down the street saw you yesterday. A little bird told me so.)
6) "My doctor is out of town, but he'll be back Wednesday. I just need enough until then."
7) You walk just fine when you don't realize you're being watched, but when I formally examine you, you ambulate like an arthritic stroke victim. My exam sometimes starts in the parking lot.
8) You forge an "ES" after the "vicodin" on the prescription. That is a felony, by the way, and I do notify the police after I get a call from the pharmacist.
9) You ask for "that shot that starts with a D." Good one.
10) "Give-away" weakness
There are more
I think you treat everybody, fakers and all. It used to (but doesn't really any more) to give a faker a dose of something. The key is that they get the workup for whatever pain they come in complaining of?
Worst headache of your life? Always gets an iv, ct scan and lp. And it should.
Back pain? Do the films.
Abd pain? Do the CT.
Because sometimes even people who are known to be druggie fakers get sick. Also, if there is no known cause to explain their pain, and especially if it's because they lost a prescription from their primary care doc, don't send them out with a script, or don't send them with more than 1 days supply, and make a note in the chart about the situation.
Eventually these people will run out of hospitals/patience/whatever and then they will either get treatment for their addiction or not.
These people have learned a terrible way to get through their lives, and it's our responsibility to take care of them in the best way we know that can limit their suffering the most until they're willing to learn some other ways of dealing with life.
My life really sucks sometimes. Having said that, I still have never met a drug seeking patient whose life I would be willing to trade for. These people have crappy lives, in general, and I'm sure they do have some genuine pain. They deserve our sympathy. That still doesn't mean that they deserve a lifetime supply of fentanyl patches or iv dilauded
I better shut up now.
First off, Scalpel - I'm sorry if I sounded a bit rude - I reread my post later and felt a little badly about it! I have been having a rough time lately, so I have been a bit snappy over some things.
And to go off of what I wrote before - I said I would post the Kip Scale that those of us with clusterheadaches go by. Well, not everybody with cluster headaches uses it - and in fact, it is not used by neurologists - but I like the scale. It came out of a need by cluster headache sufferers to understand what level of an attack each other was having. I find this to be an interesting thing - because whereas most people are striving for the theory that "nobody can rate my pain for me" - this scale sort of does that. But what our group wanted and needed was a way to understand different levels of CH hits in our own terms.
One thing I have found at the headache center is that if I were to say my clusters were an 8, then they'd look at me like I was an alien. In headache terms, clusters are always a 10. But in my own terms, based on the Kip scale, my clusters could be a whole host of different ratings, depending on the attack. But then it gets confusing when I throw in my constant migraine... There are a few, very rare times, when I have rated that a 10 - but it's a 10 on a scale for that headache. So, I know this is going a bit overboard, but for somebody who has lots of different types of pain, I almost have to give each type its own 1-10 scale. I know what my 10 is for my constant headache, and I know where I generally sit. And then I have the Kip scale for clusters. When we're talking the joint and muscle pain - whatever I rate that has nothing to do with how it compares to my headaches, so it's just in a class of it's own I guess... I don't really know. But on the times that I've had to go to the ER - I have never said that my pain was a 10, even when I thought it was. I'm too afraid of how that will stigmatize me. When I went in for my shoulder, I couldn't move it away from my side more than a couple of inches, and I was in excruciating pain that had me in tears and by the next day, even vomiting. As my dad drove me to the ER, every time we hit a bump, the shoulder spasmed and I could hardly bear it. It was one of the worst things I've ever experienced, but when they asked me to rate it in the ER - I think I said it was an 8...maybe a 9.
My thought and concern about scales that are designated, including the Kip scale, is that it serves to rate people's pain for them. What I truly believe in my heart is that every person has their own 1-10 based on their experiences. I believe that the 10 should be the worst pain you've ever personally experienced. If I view it that way, then everybody has experienced a 10 at some point in time...even though somebody else's 10 might be the next person's 5. And the reason why I stand firm that the 1-10 scale should not be standardized based on descriptors is because every person deals with pain differently. I have experienced some serious head pain, but I still work. I often find myself getting out of the car in the parking garage, and thinking, "Wow if somebody who was healthy felt like this, they'd be calling out sick..." but for me to take a sick day, I have to be much in a LOT more pain or a LOT more sick. So if I throw up in the morning, as long as I can finish getting ready afterwards, I'm still going to work. My way of dealing with it is to take all this pain and try to keep living the best I can. I have FMLA, and I have to occasionally take a day off, in spite of my pushing, but I don't think this means that my pain is not as bad as someone at home on disability. Somebody else might be at home on disability with less pain than I go to work with daily, but it is in how we deal with it. And frankly I don't feel angry or hurt over someone at home on disability while I work. I'm not bitter about that. But it's just in how we deal with it. I must deal with my pain/illness by continuing life as normally as possible. I know that I can't have a normal life, but I want to try to keep going as much as I can. What I'm trying to say, and not saying very well, is that while we each have our own levels of pain, we each additionally deal with that pain differently. Say you have a 1-10 predetermined, descriptive scale... I might not need to go to the ER until I hit a 9 on that 1-10 scale - but somebody else might need to go to the ER when they hit a 5 on it. But if you ask that person what their pain is, they would probably say a 9 or 10 - because that's how severe it feels to them. Do we then say that, "no - it's not that bad - you could be much worse..." and then tell them how much worse it could be and belittle them, invalidating their pain? That person is at their personal 9 or 10 - their personal level where they are experiencing major pain, in their minds. They might someday have worse pain and then reevaluate their scale. I think that's okay. The pain I feel today was not in my imagination 6 years ago when I first got my headache. I couldn't fathom feeling worse at the time. But I have - and I have dealt with it - and reevaluated my personal 1-10 with each experience. That's how my brain works - a constant need to compare and categorize.
I know that ER doctors and nurses (and doctors and nurses in other areas as well) feel the need to have a solid 1-10 descriptive scale so that they can compare, and effectively triage, a patient whose primary complaint (or even secondary complaint) is pain. That way, they can say, "this person rates a 5, so we must take the one who rates a 7 first.." And that's based on their own scale - the patient with a 5 might declare their own pain a 9 whereas the person with a 7 might declare their own pain a 7. I can see where it would be helpful in terms of triage, but I still believe that it is important to listen to how severe that pain is to the patient. When I went to the ER with my shoulder spasming and unable to move it, I did not want someone to tell me that the pain could be so much worse so I shouldn't rate it so high. I would have taken my good arm and punched them out...simply out of adrenaline from pain. ;)
So here's the Kip scale, for those interested: Kip scale I find it interesting - and I still use it - even if it means using a predetermined scale. But I like it - and I think for my clusters, this scale works pretty well. And then when I talk to cluster patients, I can say that last night, I had a k7, and they know exactly what I mean. But in terms of my constant migraine - it doesn't fit on this scale, and it is a lot harder to make fellow clusterheads understand that pain - because they mainly view things in terms of the Kip scale. I'm very glad that many cluster patients do not experience chronic pain outside their cluster headaches - but for those of us that do, it gets complicated.
Sorry for the length here! It remains an extremely important topic for me!
Hugz and PF wishes,
Carrie :)
One further thought: The other day, I was thinking about what everybody wrote about how pain doesn't really fit with vital signs because vital signs, if out of whack, can mean life or death - but the pain scale does not. This may be true, but I think assessing pain can help us to understand vital signs. What if you have a patient who has a heart rate of 120 and a blood pressure of 150/100? Would you give them a beta blocker if you didn't ask them if they are in pain? My vital signs actually do look like that when I have a cluster attack. I'm 26, thin, and I look healthy - and when docs or nurses see my heart rate and bp do that, they get concerned and hold me for observation. But if my pain is controlled, those signs fall back to normal a bit faster.
In neonatology, we have to go by cues to determine infant pain. One of the easiest ways to note pain in a baby is to look at their vital signs. If their heart rate is up, and they are hypertensive (comparitively), then they might be experiencing bad pain. I have watched infants have a central line placed and been in charge of giving them morphine and versed. I have to stand there and watch the vital signs, and if I note that their heart rate is climbing, then I ask the surgeon if it is okay if I give them more pain medication. There are a lot of other cues I look for, but vital signs are often where I start. The PIPP scale is based in part on variations in vital signs, including pulseox and heart rate.
And also, rating a patient's pain can give info that may be helpful during certain events - such as an MI. Patients often state that they "feel an elephant is on my chest." So we ask them to rate their pain. Some of them might just say it's an 11. We had better look into that - especially when they feel that way and also have vital signs that don't look so hot.
I realize that pain isn't as important as all of those other main signs, but I think the whole idea of the push to make "pain the 5th vital sign" was more to put it in the front of our minds and to make sure that pain was addressed. No, it doesn't have to be in the front of the line, but it used to be all-too-often ignored, and this campaign has made it something that many more people are in tune with now.
Take care,
Carrie :)
Blocked out of Blogger, for days on end.
Is there a scale for blogging withdrawl? Is that its own kind of pain? Please can I circle a frowny face?
Roy, ClinkShrink :rescue me.
Dinah,
I'm sure we could adapt the neonatal abstinence syndrome scale for blogging withdrawal...with some adjustments. ;)
Threaten them with starting your own blog so that you can cure your blogging withdrawal...that should get them to act more quickly to help you get back into blogger! ;) haha
Hang in there!! We miss your posts!
Carrie :)
Post a Comment